The Power of Listening to Patients: Improving Healthcare Through Technology and Compassion
The following is a guest article by Dr. Gary Rothenberg, DPM, Director of Medical Affairs at Podimetrics and Associate Professor of Internal Medicine at the University of Michigan, and Jordan Munson, RN, MSN, Director of Patient Experience at Podimetrics In an era where healthcare technology is advancing at an unprecedented pace, one truth remains evident: […]

The following is a guest article by Dr. Gary Rothenberg, DPM, Director of Medical Affairs at Podimetrics and Associate Professor of Internal Medicine at the University of Michigan, and Jordan Munson, RN, MSN, Director of Patient Experience at Podimetrics
In an era where healthcare technology is advancing at an unprecedented pace, one truth remains evident: Technology alone will not solve the challenges facing our healthcare system. When managing chronic conditions like type 2 diabetes, genuinely listening to patients is the key to improving care and reducing disparities. At a time when healthcare professionals and policymakers are increasingly turning to digital tools, it’s essential to remember that patient engagement and human connections are just as critical as the technology itself.
Our recent Medicaid Survey Report reveals compelling insights into the lived experiences of patients with type 2 diabetes, particularly those enrolled in Medicaid programs. Type 2 diabetes affects 1.6 million Americans, and Medicaid/dual beneficiaries face a disproportionate burden due to systemic barriers like socioeconomic challenges and limited access to resources. The survey shows a growing demand for better tools, with 86% of respondents wanting more ways to connect with their care teams.
This highlights an important question: How can healthcare systems improve patient outcomes using technology while addressing the human factors influencing health?
A Snapshot of the Medicaid Survey Insights
The survey had responses from over 1,000 Medicaid beneficiaries living with type 2 diabetes, offering a deeper understanding of their struggles and needs. Some key insights include:
- 86% want their health plans to cover more tools to stay connected with their care team
- 78% believe their health plans should offer additional digital resources to manage their condition
- 66% are willing to try new clinical programs or tools to support their care
- Nearly 9 in 10 beneficiaries believe remote patient monitoring (RPM) devices should be paired with consistent clinical support
These findings reveal that patients are not just looking for more digital solutions but for tools that come with personalized support, recognize their social challenges, and actively involve them in their own care.
Remote Patient Monitoring: A Key Component of the Solution
Remote patient monitoring (RPM) is often heralded as a game-changer in chronic disease management. RPM allows healthcare providers to monitor patients remotely, empowering them with data to make timely, informed decisions. Yet, technology is only as good as the way it’s implemented. The Medicaid survey revealed a fundamental truth: patients are open to RPM, but they require consistent, compassionate care to go along with it. This combination of connecting patients, providers, and data is what leads to real improvement in patient outcomes.
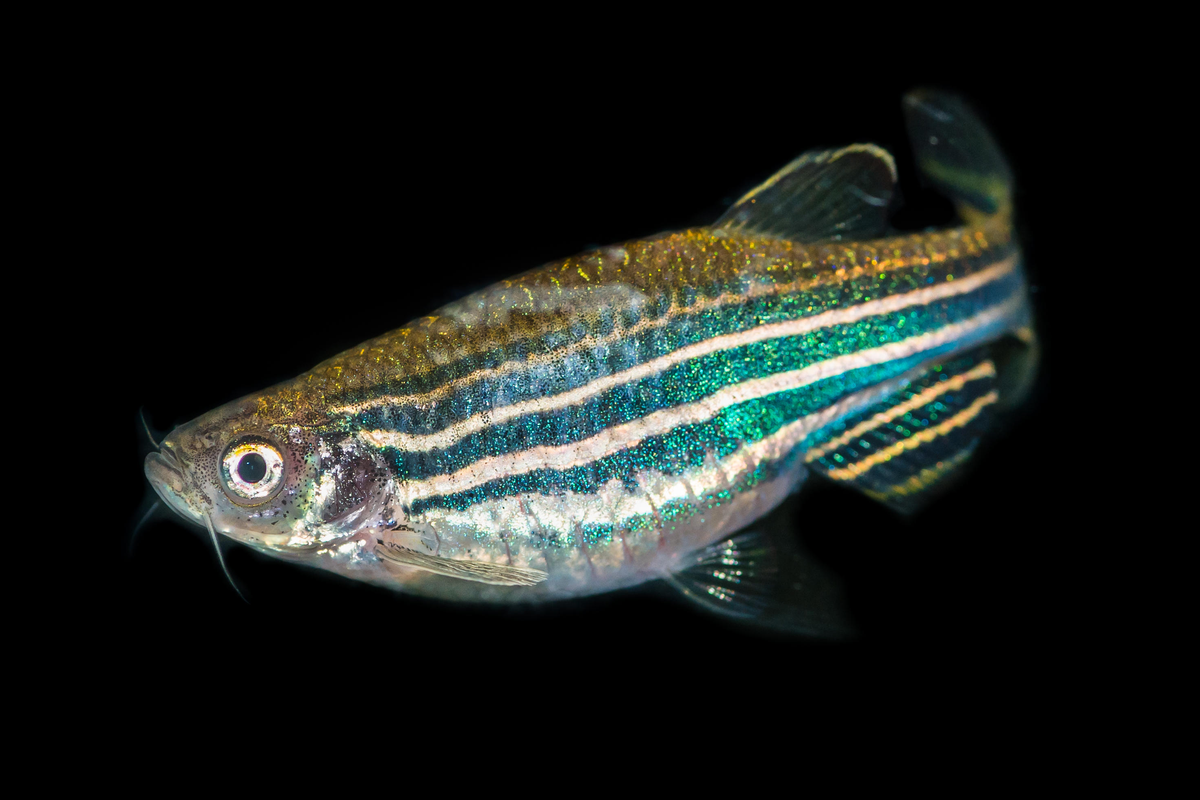
For example, in our work with Podimetrics, we’ve implemented the SmartMat Program for diabetic foot ulcer (DFU) prevention—an innovative RPM tool that’s been designed with ease of use and patient-centricity at its core. Patients simply step on the mat for 20 seconds, and critical health data is transmitted to their care team without needing Wi-Fi or smartphones. The results are striking: 88% of patients report that the SmartMat is easy to use, and adherence rates exceed 86%. This is just one example of how thoughtfully designed technology can drive positive outcomes.
However, RPM is not the only factor that contributes to success. The combination of technology with continuous support, feedback, and trust-building delivers the most impactful results.
Lessons from Success Stories: What Works and Why
From these insights, we can identify a few critical lessons for healthcare professionals and organizations looking to implement digital tools effectively:
- Choose Tools with Patients in Mind: Healthcare providers must focus on the needs, preferences, and challenges of their patients; by listening to feedback and ensuring technology fits seamlessly into daily life, providers can make tools effective, accessible, and user-friendly
- Support Patients and Providers Simultaneously: Successful RPM programs provide ongoing, personalized support to patients and providers — many survey respondents believe regular touchpoints with their care team would improve their health outcomes; this support is key—patients need reassurance and guidance, while providers need efficient tools that simplify workflows and improve care delivery
- Continuous Process Improvement: It’s important to remember that healthcare tools must evolve alongside patients’ needs; whether from patients or providers, continuous feedback ensures that tools remain relevant and effective — this process of iteration is key to ensuring that digital programs can drive long-term success and better patient outcomes
Shifting the Focus: From Technology to Human Connection
While technology can certainly be crucial in improving healthcare, it’s essential to remember that patients are more than just data points—they are human beings with unique stories, needs, and barriers. Addressing the systemic challenges that Medicaid/dual beneficiaries face, such as food insecurity and transportation, cannot be solved through technology alone. Healthcare providers must adopt a holistic, compassionate approach to care where human connection and empathy are prioritized.
When technology is paired with ongoing, personalized support, it has the power to reduce health disparities and improve care outcomes for underserved populations. This approach is not just about digital innovation—it’s about using technology to build trust, engage patients in their care, and meet them where they are.
A New Model for Healthcare
The future of healthcare will undoubtedly involve more digital tools, but the success of these tools depends on how well they integrate into patients’ lives. As we continue to innovate, it’s essential that healthcare professionals remain focused on what truly matters: listening to patients, addressing their needs, and creating a system that values both technology and compassion.
For healthcare organizations looking to improve outcomes for patients with chronic conditions like type 2 diabetes, the solution lies in blending digital innovation with human-centered care. By doing so, we can create a more equitable healthcare system, one that works for everyone, no matter their challenges or circumstances.
 About Dr. Gary Rothenberg, DPM
About Dr. Gary Rothenberg, DPM
Dr. Gary Rothenberg is a board-certified podiatrist with over 20 years of experience in academia, clinical practice, and research, specializing in preventing diabetes-related lower extremity complications. He serves as Director of Medical Affairs at Podimetrics and Associate Professor of Internal Medicine at the University of Michigan.
 About Jordan Munson, RN, MSN
About Jordan Munson, RN, MSN
Jordan Munson is a seasoned nurse with over a decade of experience in direct patient care and a deep commitment to patient advocacy. She combines her clinical knowledge with data-driven insights to shape the patient experience, advocating for exceptional care as the Director of Patient Experience at Podimetrics.



















































































































![[Industry Direct] PHI Studio & Agog Are Seeking Immersive Artists for a Four Week Residency Program](https://roadtovrlive-5ea0.kxcdn.com/wp-content/uploads/2025/05/phi-immersive-residency-2-341x220.jpg?#)