Most Impactful Digital Health and IT Innovation Projects on Healthcare Organizations
There are a lot of digital health and IT innovation projects currently happening in the world of healthcare. We were curious to see what projects people thought would have the most impact on healthcare organizations. So we reached out to our brilliant Healthcare IT Today Community to ask just that! What digital health and IT […]

There are a lot of digital health and IT innovation projects currently happening in the world of healthcare. We were curious to see what projects people thought would have the most impact on healthcare organizations. So we reached out to our brilliant Healthcare IT Today Community to ask just that! What digital health and IT innovation projects do you see having the most impact on healthcare organizations? Why? The following are their answers.
Julie Stegman, Vice President, Health Learning & Practice at Wolters Kluwer Health
VR technology can provide case-based or scenario-based learning—invaluable for the development of critical thinking skills, communication, and problem-solving in the next generation of healthcare professionals. Depending on where a student or practitioner is located, these virtual encounters may also be more diverse and challenging than what they would see in their local hospital, offering new opportunities for real-life education and refining clinical decision-making with high acuity cases and a varied patient case load. The availability of complex clinical scenarios in a virtual setting allows students, regardless of their physical location, to gain experience with more unique cases than they might otherwise see in their classroom education or local clinical training, which can lead to a more highly skilled workforce in these areas.
Kevin Ritter, EVP of the dbMotion solution at Altera Digital Health
Large language models (LLMs) will drive the next evolution of AI in healthcare by making sense of vast quantities of data. Healthcare organizations will have the ability to bring real-time analytics to the point of care so providers can make more informed care decisions without hunting for relevant information across fragmented medical records. As care delivery becomes more efficient and effective, it will also become more proactive, rather than reactive. The combination of LLMs and predictive analytics will give providers the ability to identify at-risk patients and apply preventative interventions. This will enable true healthcare, rather than “sickcare,” elevating experiences for patients and providers alike.
Lora Sparkman, MHA, BSN, RN, Partner, Clinical Solutions at Relias
Technology is transforming healthcare training, making learning more engaging, efficient, and effective. While VR is well-established in fields like emergency services and aviation, it offers many positive benefits when applied to training the healthcare workforce. By replicating real-life scenarios, VR allows healthcare professionals to practice decision-making in immersive environments that reflect everyday challenges.
Unlike traditional training, VR provides real-time feedback that reinforces learning and changes behavior. For instance, in infection prevention training, they not only practice proper hand hygiene but also see the consequences of missed steps, creating a visceral and memorable experience proven to improve compliance. This innovative, immersive training method is shown to enhance retention, improve preparedness, and ultimately lead to better patient outcomes — all in 15-minute learning sessions.
Oren Nissim, Co-Founder and CEO at Brook.ai
AI’s most profound impact on healthcare isn’t happening within hospital walls, but in patients’ living rooms. By intelligently blending AI capabilities with human clinical expertise, we’re creating a new paradigm of continuous, adaptive care that extends far beyond traditional episodic interactions. These intelligent systems can analyze patterns across biometric data, behavioral indicators, and environmental factors to identify subtle changes in patient condition before they become critical events. This allows remote clinical teams to intervene at precisely the right moment with the right level of support.
The real innovation isn’t just in the technology itself, but in how it enables a fundamentally different relationship between patients and providers – one where care becomes ambient, preventive, and deeply personalized. As these hybrid AI-human care models mature, we’re seeing remarkable improvements in chronic disease management, reduced hospital readmissions, and significantly enhanced quality of life for patients who can now receive sophisticated clinical monitoring while maintaining their independence at home.
Ahzam Afzal, Co-Founder and CEO at Puzzle Healthcare
As hospitals and health systems continue to face high rates of readmissions across care transitions from hospitals to skilled nursing facilities and home care, innovative technologies such as remote patient monitoring and patient flagging are improving outcomes in post-acute care by enabling care providers to more effectively monitor patients post-discharge. Manual methods of tracking patients can be labor-intensive and prone to human error.
With this, patient monitoring and flagging technologies are emerging as an innovative solution to catching signs of deteriorating health early on. This enables care providers to better prioritize patients’ needs and ensures that all patients receive continuous, high-quality care when transitioning through care environments and stages of recovery.
By integrating innovative patient monitoring and tracking technologies, healthcare facilities can establish and enhance care models that address immediate health concerns. Simultaneously, they will foster better health outcomes for patients and reduce the overall burden on healthcare systems by cutting readmission rates and bolstering cost savings.
Eric Prugh, Chief Product Officer at Authenticx
Contact centers are a prime area of innovation in healthcare. It’s likely that every single issue you are trying to solve for as a business has come through your contact center in one way or another. Opportunities with AI are transforming the idea that contact centers are simply “performance management” and instead a place of insights that impacts your entire enterprise and customer experience.
Training AI models with industry data is the key to improving outcomes. From unlocking customers’ needs, problems, and gratitude to providing clear-line, actionable call center metrics and operational insights to improve the CX, these AI-driven projects can help healthcare leaders meet positive patient outcomes (good health, good service) alongside positive business outcomes (retention, good scores, bottom line). Identifying these trends faster and with greater clarity enables organizations to turn insights into actionable strategies that drive better patient outcomes and business results.
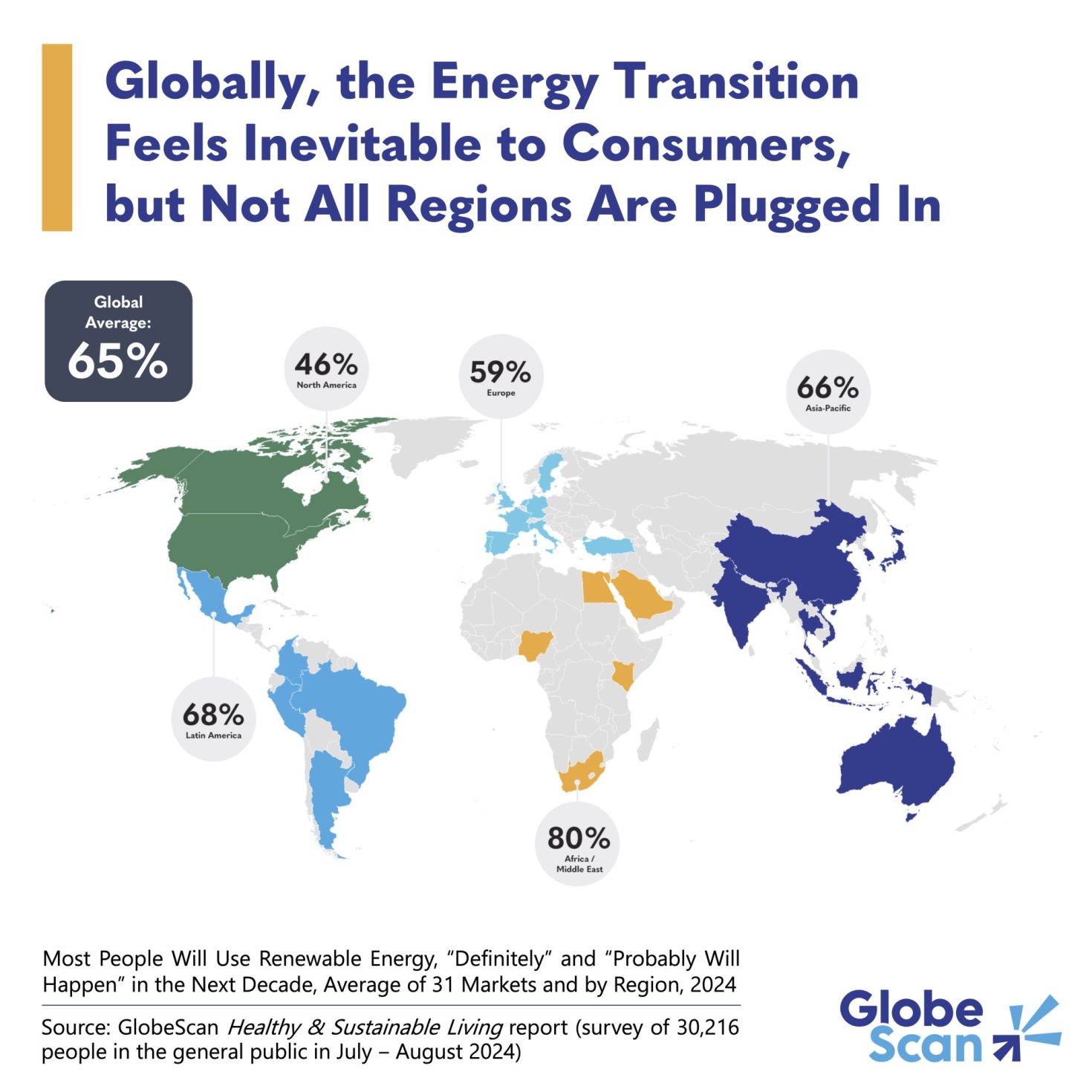
Krista Bowman, Managing Director, Head of Healthcare and Life Science at Further
Personalized medicine has shifted from a “one-size-fits-all” model to a data-driven, patient-specific approach. Population health initiatives aimed at combating chronic diseases and enabling early detection have evolved with advances in data analytics and AI. These advancements now support targeted therapies tailored to unique genetic and clinical profiles, ultimately improving survival rates. Breakthroughs in gene therapy and CRISPR-based treatments activate precise genetic modifications to potentially cure inherited conditions and certain cancers. As medical insights evolve, addressing challenges like data quality, privacy, AI bias, and the need for clinical validation is paramount. Continued innovation and collaboration will unlock even greater possibilities and improve outcomes globally.
Robin Ntoh, VP of Aesthetics at Nextech
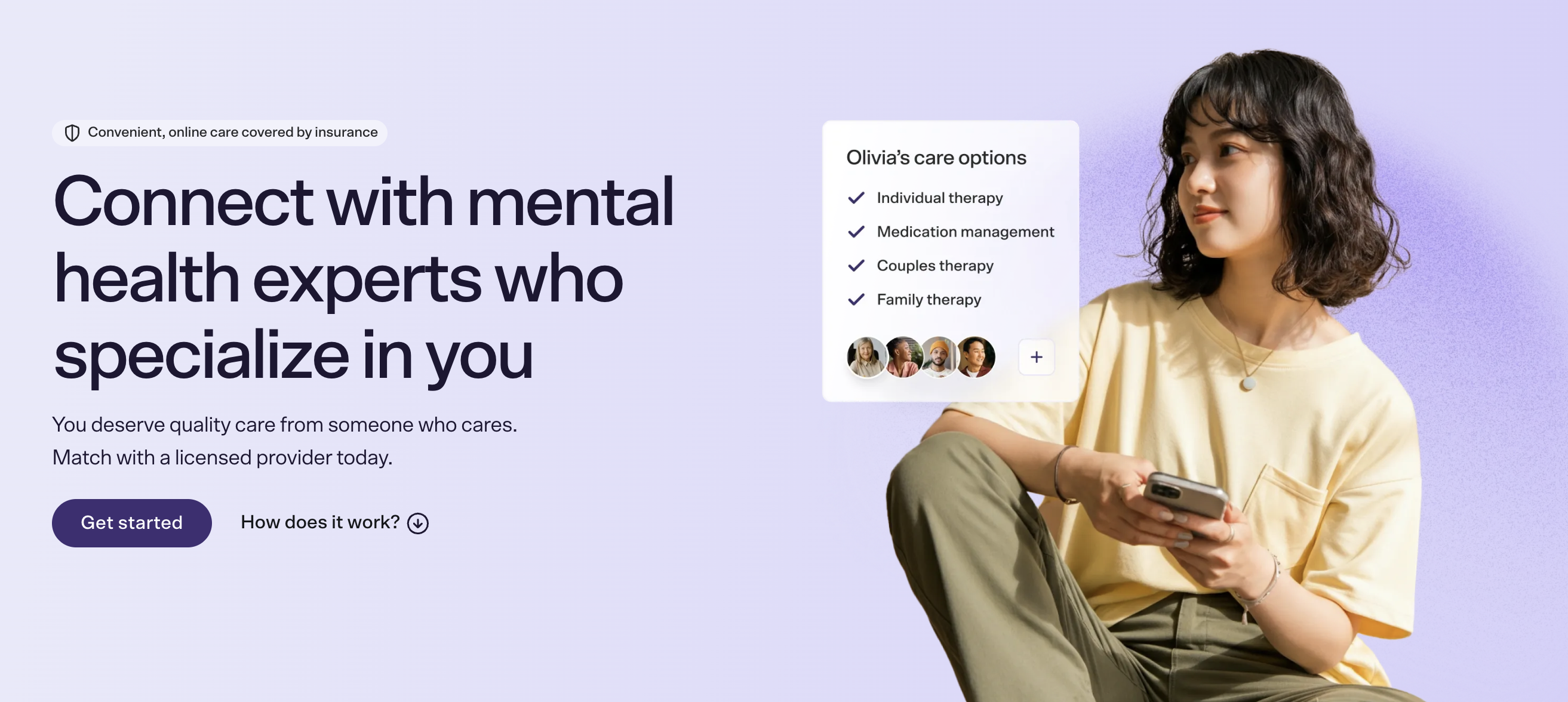
Patients today expect a personalized healthcare journey at every touchpoint, from their first visit to a provider’s website to their time in the exam room and beyond. As technology becomes more integrated into daily life, healthcare must meet these rising expectations — every interaction can enhance or diminish the patient experience.
The digital innovations with the most impact on care delivery are EHR and practice management tools, including RCM and payment functions, that are designed with providers and patients at the forefront. It is critical, especially in specialty medicine, that practice managers and clinicians have the right information available to support positive provider-patient interactions. I am also passionate about technology that caters to diverse patient populations across all generations. As health leaders, we must adapt and ensure all patients from Gen Z to Baby Boomers have access to positive experiences and outcomes.
Chris Gallagher, CEO at Access TeleCare
There’s a growing appetite among healthcare organizations for digital health solutions that solve long-standing problems such as provider availability, or lack thereof, and expenses associated with providing care. One of the innovations healthcare organizations are increasingly turning to address their most pressing issues is telemedicine, particularly in the acute hospital setting.
Historically, hospitals and health systems have had few options to address the growing issue of a lack of physicians able to provide high-quality patient care. In fact, the hospital staffing shortage has become so problematic that the US is on track to reach a “dangerous threshold” of hospital bed occupancy in the next several years. Solutions – from inadequate (and dangerous) staffing levels, to bringing in locums, to burning out existing providers with earnings incentives – have been short-term and less than ideal. Over the past decade, hospitals have begun to take a fresh approach, turning to virtual care options first, supplemented by in-person care. Hybrid care models prioritize the delivery of quality patient care. The method(s) of care delivery are secondary.
Using telemedicine as the cornerstone of a hybrid approach allows facilities to treat more patients and optimize their capacity, enabling hospitals to operate more efficiently. It also shrinks revenue leakage and promotes cost savings.
In the case of one rural Indiana hospital that was unable to appropriately staff its ICU, working with a telemedicine partner allowed the facility to open a two-bed virtual ICU. Doing so increased the number of surgeries the facility was able to perform and reduced transfers out of the hospital. Beyond positive financial outcomes, the hospital experienced enhanced patient satisfaction. Using telemedicine to increase its capacity – and therefore, access to timely specialty care – another hospital doubled the number of annual visits to its ED in just a few years.
Wes Cronkite, Chief Technology & Innovation Officer at TruBridge
Revenue cycle automation and AI-driven analytics are two important innovations that save hospitals valuable time, money, and resources. Automating financial processes like cash posting and claims management reduces administrative burden, minimizes errors, and ensures steady cash flow – critical advantages as providers grapple with increased costs and tightened budgets. Real-time analytics provide insights into payer behavior and reimbursement trends, allowing hospitals to proactively prevent denials and boost revenue capture.
AI frameworks continue to improve through initiatives like the Trustworthy & Responsible AI Network (TRAIN), which focuses on ethical and unbiased AI development and deployment. These innovations continue to enhance accuracy; however, successful integration depends on clear governance frameworks, peer review, rigorous bias testing, and proper staff training. Strategic implementation of these innovations strengthens financial resilience and allows staff to refocus on high-touch priorities.
Ben Maisano, SVP Strategy at Tendo
One of the most impactful digital health innovations is the expansion of direct-to-employer and direct-to-consumer care models through marketplace-driven platforms. These solutions create new growth channels for healthcare organizations while streamlining financial operations by enabling upfront bundled payments—eliminating prior authorizations, patient collections, and claims delays or denials. For employers and consumers, integrating transparent, fixed-cost care into benefit design alongside traditional insurance improves access to high-quality providers while reducing financial complexity. As healthcare shifts toward greater efficiency and transparency, these models are poised to play a critical role in reshaping care delivery and payment structures.
So many great ideas here! Huge thank you to everyone who took the time out of their day to submit a quote! And thank you to all of you for taking the time out of your day to read this article! We could not do this without all of your support.
What digital health and IT innovation projects do you see having the most impact on healthcare organizations? Why? Let us know over on social media, we’d love to hear from all of you!