AI and Decentralized Trials: A New Era in Drug Development
The following is a guest article by Matt Noble, Head of Patient Experience at Medidata The decentralized clinical trial (DCT) model has been around for almost fifteen years, with Pfizer pioneering the first fully decentralized study in 2011, and adoption accelerating significantly following the onset of the COVID-19 pandemic in 2020. The clinical research landscape […]

The following is a guest article by Matt Noble, Head of Patient Experience at Medidata
The decentralized clinical trial (DCT) model has been around for almost fifteen years, with Pfizer pioneering the first fully decentralized study in 2011, and adoption accelerating significantly following the onset of the COVID-19 pandemic in 2020. The clinical research landscape is currently undergoing a profound transformation, driven by the increasing employment of decentralized clinical trials. Traditional clinical trial models, which rely heavily on centralized study sites and in-person participation, have long been hindered by geographic, logistical, and financial barriers. These challenges have slowed patient recruitment and participation, limited trial diversity, and delayed access to life-saving treatments.
The pandemic showed us that DCTs can change this dynamic, leveraging digital health technologies to bring trials directly to participants. By incorporating remote monitoring, point-of-care testing, and AI-powered analytics, DCTs are improving patient accessibility, engagement, and data quality while accelerating trial timelines. As regulatory bodies worldwide provide clearer guidance on decentralized methodologies, the future of clinical research is becoming progressively decentralized, data-driven, and patient-centric.
Understanding Decentralized Clinical Trials
DCTs represent a fundamental shift in how clinical trials are conducted. Unlike traditional trials that require frequent in-person visits to designated research sites, DCTs utilize a combination of telemedicine, home-based diagnostics, wearable devices, and remote monitoring platforms. This approach minimizes patient burden while ensuring continuous data collection and trial oversight.
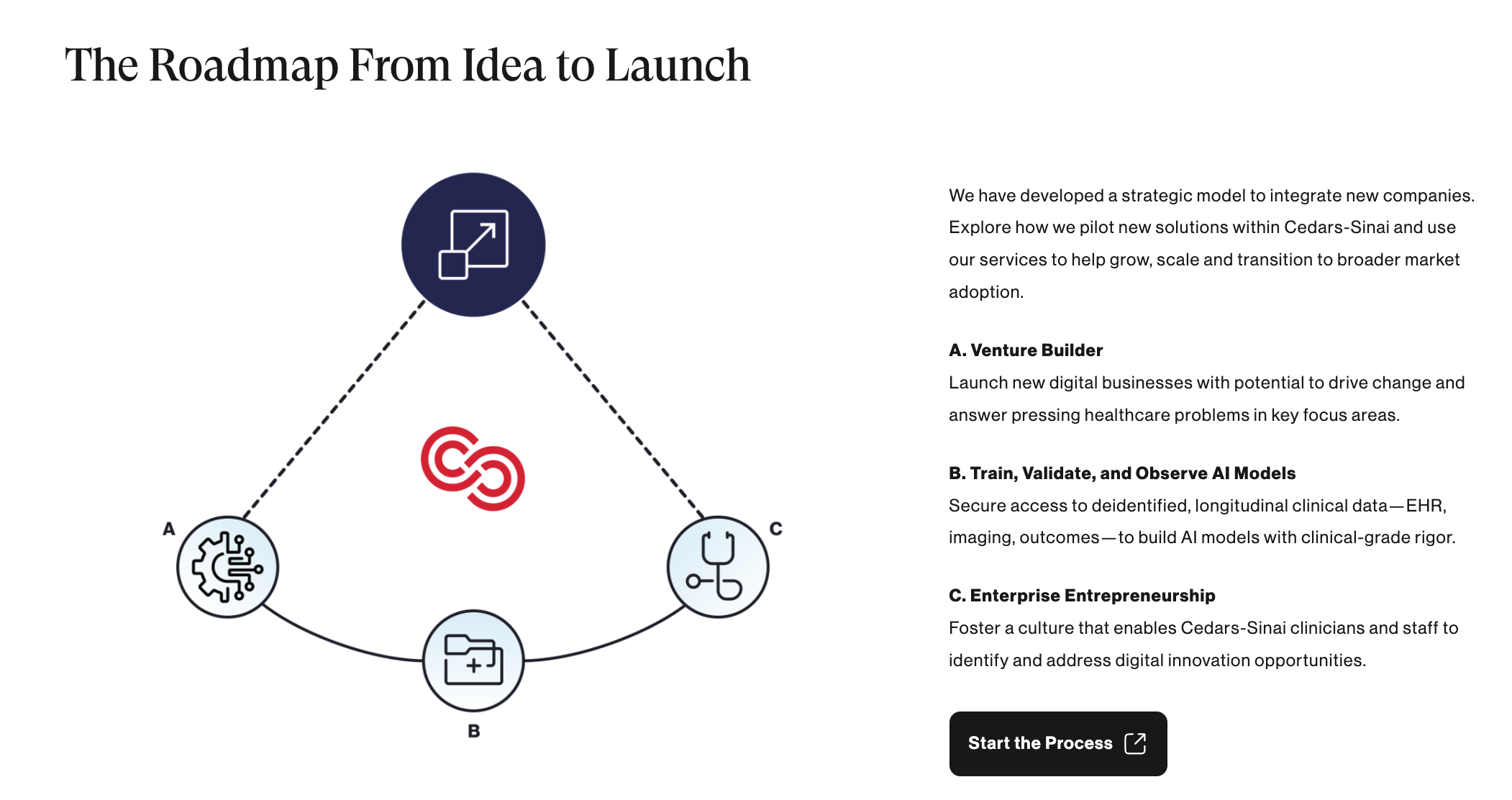
AI is playing a pivotal role in DCTs, enhancing study design and improving patient recruitment, data collection, and analysis. Advanced machine learning models help identify suitable participants by analyzing electronic health records (EHRs) and other real-world data sources. AI-driven automation ensures efficient trial execution, detecting anomalies in real time, improving data integrity, and mitigating risks associated with patient attrition.
Overcoming Traditional Trial Challenges
Historically, clinical trial participation has been geographically constrained, favoring patients who live near major research centers. This has resulted in significant underrepresentation of diverse populations, including racial and ethnic minorities, rural communities, and individuals with rare diseases. DCTs eliminate these barriers by enabling participation regardless of location. AI-powered recruitment platforms proactively identify eligible participants from broader and more diverse populations, ensuring trials better reflect real-world patient demographics. In fact, one study found that DCTs “contributed to faster-than-planned enrollment timelines” and a significantly higher proportion of Asian participants compared to the benchmark.
For rare disease research, where patient pools are inherently small and geographically dispersed, DCTs are particularly transformative. They reduce the need for frequent travel and, in some cases, eliminate the need for patient relocation, making trial participation more feasible and reducing dropout rates.
Enhancing Data Quality and Trial Efficiency
Remote monitoring and digital tools embedded within DCTs significantly improve data accuracy and reduce delays. Wearable devices continuously track physiological parameters, providing real-time insights that enhance trial oversight. AI-powered analytics processes this vast influx of data, detecting potential issues before they escalate and enabling swift intervention.
The integration of point-of-care testing (POCT) in DCTs is another game-changer. The COVID-19 pandemic accelerated advancements in POCT, highlighting the feasibility and demand for at-home diagnostic solutions. Today, POCT allows patients to perform rapid tests in their own homes, such as glucose monitoring for diabetes or antigen tests for respiratory viruses like COVID-19, with results seamlessly transmitted to research teams. This reduces the reliance on in-person visits while maintaining high standards of data reliability.
EHR integration further enhances data accuracy within DCTs, ensuring a comprehensive and continuous flow of patient information. By pulling relevant clinical data directly from healthcare systems, researchers can gain deeper insights into patient responses while reducing reliance on self-reported data. This streamlined access to high-quality data improves the efficiency of the study, which, in turn, accelerates trial timelines and helps sponsors bring therapies to market faster for patients who need them most.
Technology-Driven Patient Engagement and Retention
One of the longstanding challenges in clinical trials is patient retention. Traditional trials often experience high dropout rates due to the inconvenience of travel, scheduling conflicts, and the burden of repeated site visits. DCTs alleviate these challenges by incorporating personalized engagement strategies powered by AI. These personalized engagement strategies use machine learning to tailor support to each participant, such as by analyzing each patient’s habits and sending medication or appointment reminders at times they’re most likely to respond. By anticipating patient needs and removing barriers to participation, AI-driven engagement helps maintain involvement and reduces dropout rates.
Telemedicine platforms facilitate regular patient check-ins, reducing the need for in-person appointments. Automated reminders, gamification, and personalized digital communication enhance protocol adherence, keeping participants actively engaged. Additionally, AI-driven chatbots provide real-time support, answering patient questions and addressing concerns, further fostering retention.
Wearable devices complement telemedicine by continuously capturing biometric data, alerting researchers to any deviations from expected health trends. This real-time feedback loop not only strengthens patient engagement but also improves safety monitoring, allowing clinicians to intervene proactively when necessary.
Regulatory Landscape and Future Outlook
As the adoption of DCTs accelerates, regulatory agencies are refining guidelines to support these methodologies. The FDA and global regulatory bodies are increasingly recognizing the value of decentralized approaches, offering frameworks that balance innovation with patient safety and data integrity.
Decentralized clinical trials are ushering in a new era of drug development, breaking down barriers to participation, improving data integrity, and accelerating time-to-market for life-saving treatments. AI, POCT, and wearable technologies are at the forefront of this transformation, driving unprecedented efficiency and inclusivity in clinical research. As the industry continues to embrace these advancements, stakeholders must remain committed to regulatory compliance, data security, and patient-centric innovation. By doing so, we can unlock the full potential of DCTs, ensuring that groundbreaking therapies reach the patients who need them most, faster and more equitably than ever before.
 About Matt Noble
About Matt Noble
Matt Noble is the Head of Patient Experience at Medidata. As part of his job function, he oversees a suite of powerful patient-facing solutions, including eCOA, eConsent, and Decentralized Clinical Trial (DCT) capabilities. Previously, as Senior Vice President of Product Management, Matt led the product development efforts for Patient Cloud technology since the initial launch of Patient Cloud eCOA, the industry’s first BYOD (bring your own device), app-based solution in 2014.
Noble has over 17 years of experience building and leading complex B2B software products across both the life sciences and financial services industries. Prior to joining Medidata, Noble was a Vice President at Goldman Sachs, focused on building financial pricing and reporting software.