Reducing Denials and Improving the Success Rate of Claim Reimbursements
Careers in the healthcare space are not for the weak — they’re often overworked, underpaid, and can regularly face harassment and/or violence from their patients. And despite all of that, people still have this as their dream career. This is because the ones that do choose this as their career don’t do it for the […]

Careers in the healthcare space are not for the weak — they’re often overworked, underpaid, and can regularly face harassment and/or violence from their patients. And despite all of that, people still have this as their dream career. This is because the ones that do choose this as their career don’t do it for the money or the thanks; they do it because they want to be able to help take care of others.
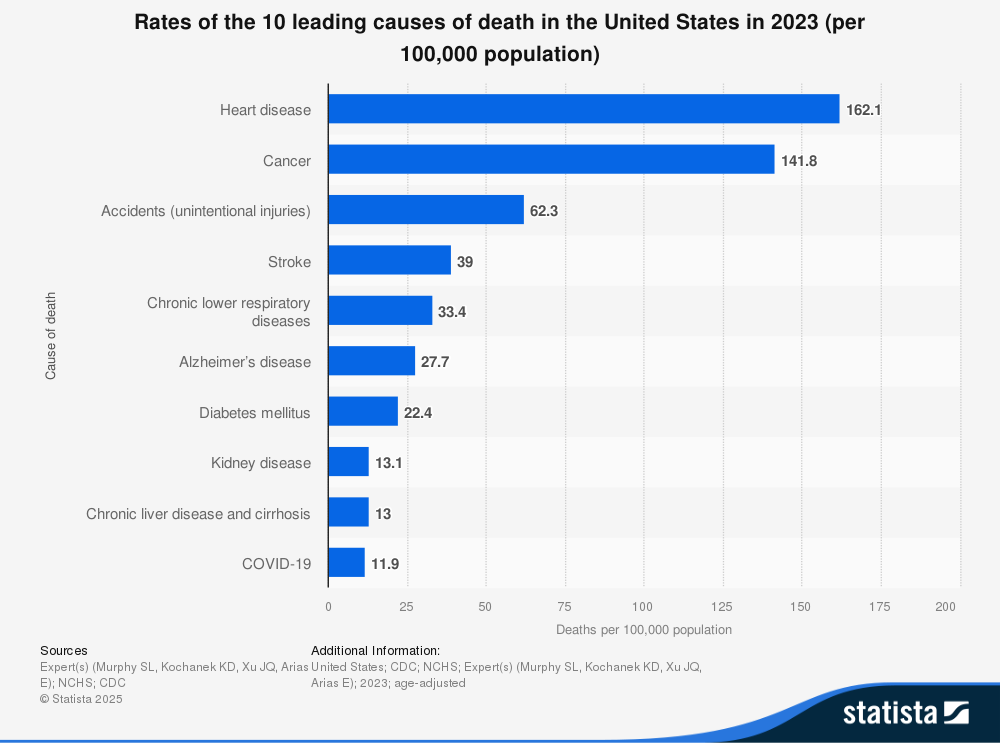
A very noble answer, however, the money must be there in order for their work to continue. Without receiving the proper compensation for the care that you have provided, your organization will simply lack the funds necessary to continue to care for your patients. This is a task that becomes more complex with the rising costs of care, the aforementioned overworked staff making an error that results in a denial, and the increasing reluctance of others to fully reimburse your claims.
We reached out to our incredible Healthcare IT Today Community with this very important topic to learn more on how to best navigate this situation. We asked — how can healthcare IT help providers reduce denials and improve the success rate of claim reimbursements? The following is what they had to share.
Navesh Kandiyil, MD, MBA, FACHE, Senior Vice President, Coding Commercialization at IKS Health
Current silos in denials need to be broken down by creating visibility between the various work streams throughout the process. When data from across the system is in one place, better analytics are created, empowering operational leaders to drive better results with better clarity. By creating and developing the appropriate integrations, visibility is improved. Creating a preactive approach to problems instead of a retroactive approach improves the success rate of claim reimbursements.
Kali Durgampudi, CEO at Apprio
Studies show that 86 percent of denied claims are due to minor and easily preventable errors. With automation and machine learning, you can avoid those errors. Even better, as process data is accumulated and mined, you can predict errors before they happen, identifying which claims are most likely to be denied and address concerns before you submit them.
Monte Sandler, Chief Operating Officer at WebPT
One of the most valuable strategies I’ve seen applied to the revenue cycle is the “shift left” approach, encouraging developers and operators to address the root causes of claim exceptions (rejections, denials, and unpaid AR) as early in the process as possible. By doing this, the downstream work involved in resolving these issues is eliminated, significantly optimizing net collection rates and lowering the overall cost to collect.
Joe Dore, President at USBenefits Insurance Services
The truth hurts! While stop-loss carriers are at the tail end of the financial transaction of self-funded employer plans, the healthcare industry can further stabilize their revenue stream and improve timely payments by disclosing their contract terms and costs. Transparency, fairness, and consistency are the key. The best way to describe the healthcare pricing from a consumer’s perspective? Would you patronize a restaurant that did not disclose its prices, charged every customer a different price, forced the customer to negotiate the final bill regardless of the outcome, leaving the customer feeling helpless with a bad taste in their mouth? From a financial standpoint, it creates uncertainty that makes it difficult to plan, budget, or trust the process — an unpredictable and risky environment that no other industry would tolerate.
David Schweppe, Chief Analytics Officer at MedeAnalytics
No one can perfectly predict the future, but with mountains of data, you can come pretty close. Healthcare has a mountain range of data, and millions of decisions are made and predicted every day with it. Providers tapping into that data, specifically payer data, can predict and prevent denials before claims are submitted. And by prioritizing high-dollar, high-probability claims, when denials do occur, healthcare workers can focus their efforts where they’ll have the greatest impact.
Ritesh Ramesh, CEO at MDaudit
Healthcare IT needs to focus on integrating denials data across disparate billing systems in a centralized location before they can deploy powerful technologies like AI to unlock value in that data. Once data is centralized, AI can be deployed to find anomalies and outliers in the denials data to then take action on them by leveraging AI-driven workflows and automation. Healthcare IT should modernize their talent and technology staff in Cloud, AI, and Analytics, moving past systems of record like EHR and Clinical systems to capitalize on unlocking value and insights from their unstructured data.
Cheryl Taylor, Vice President, RCM Advisory at Cognizant
Beyond simply managing denials after they occur, healthcare organizations must shift left — addressing issues before claims are submitted. Medical and billing policies can be complex and ambiguous, making it difficult to pinpoint corrective actions. Technology can proactively flag potential errors before claims are processed, providing users with comprehensive information to handle claims accurately the first time. This preventative approach significantly reduces rework and revenue leakage. Utilizing Agentic AI to support RCM teams throughout the entire revenue cycle will be crucial for healthcare entities to not just survive but thrive in an increasingly complex reimbursement landscape.
John Bou, Co-Founder and President at Modio Health
Revenue cycle management (RCM) is extremely complex, and even well-run medical practices can run into unforeseen challenges and leave money on the table. Innovative health technology tools can be a game-changer here. More specifically, one of the most effective ways to improve RCM outcomes is to modernize your provider credentialing process. What was once a slow, manual process can be transformed with the right digital tool. For example, AI can help automate repetitive, high-friction tasks in provider credentialing, not only reducing administrative burden but also accelerating time-to-revenue, making it a smart first step toward a more efficient revenue cycle.
A good place to start is to evaluate your credentialing process—if it’s still manual (i.e. sticky notes and spreadsheets) and error-prone, it’s time to explore AI and digital tools that can streamline operations, reduce delays, and protect your bottom line. Modernizing this single piece of the revenue cycle can unlock major gains in efficiency and financial performance.
Sandhya Ravi, Principal Product Manager at AGS Health
Data analytics and predictive modeling have become fundamental components of modern denial management. By assisting revenue cycle leaders with intuitive and interactive data management tools, healthcare IT can help with monitoring denial trends and root cause analysis, as well as tracking the effectiveness of remediation strategies. Predictive modeling can help providers avoid denials altogether or assist in prioritizing denials that occur with propensity to overturn scoring. These same predictive models are also proving to be highly effective with patient payments.
Additionally, introducing intelligent automation throughout the revenue cycle can help eliminate potential human error, delivering greater accuracy, consistency, and compliance. This can be particularly beneficial in your mid-cycle operations, including CDI, coding, and auditing activities, where many clinical and coding-related denials occur. Tools like AI-powered clinical documentation improvement software, computer-assisted coding, autonomous coding, and code auditing software can analyze charts and either recommend or produce final codes. Newer technology also allows clinical appeal work, a traditionally labor-intensive function, to be streamlined and largely automated, freeing clinicians from non-patient work. With a fully integrated platform, these automation tools can even assist with cross-departmental collaboration, improving physician queries and audit trails. The net result is shorter claims processing times, fewer denials, and more accurate reimbursements.
Combining analytics and predictive models, intelligent automation, and human expertise currently represents the apex of revenue realization. By combining these assets, revenue cycle leaders can rapidly analyze real-time performance data and free up time for their experienced team members to identify creative corrective actions.
Jennifer Bishop, Vice President of Product Content at Health Catalyst
To gain real-time insights into financial performance and key Revenue Cycle Management (RCM) metrics, health systems should leverage a combination of advanced tools and strategic practices. This includes implementing a revenue integrity solution by choosing a platform that ensures access to current coding information and up-to-date peer pricing data, aligned with the latest billing and regulatory guidelines, helping to prevent costly errors and support accurate reimbursement. Health systems should also collaborate with a proactive technology partner who can provide timely updates on policy changes and offer guidance on adapting RCM practices, ensuring ongoing compliance and optimal system performance.
Additionally, integrating and streamlining RCM data by unifying information across the revenue cycle enhances visibility into cost and performance metrics, allowing clinical and administrative teams to work more efficiently and focus on delivering high-value patient care. By adopting innovative technologies and building strong vendor relationships, healthcare organizations can improve billing accuracy, increase operational transparency, and achieve more consistent financial performance.
Sajeed Chowdhury, Director, Transformation and Innovation Services at Nordic
Healthcare IT reduces denials and boosts reimbursement by automating eligibility checks, ensuring coding accuracy, and flagging issues before submission. Health systems can use predictive analytics tools to forecast the overall cost of care, resource utilization, and payment risks. This creates an opportunity for improving organizational finances in today’s turbulent market.
Christiane Freese-Jones, VP, Strategic Product Management at Nordis Technologies
Improving patient billing and payments offers a major opportunity for shoring up provider financial health. While much effort and attention has focused on the financial toll from rising claim denials, research shows over half of hospital bills go unpaid. To increase patient collections, leading healthcare organizations are transforming patient billing and payment processes by prioritizing digital solutions that deliver the convenience, speed, and ease of use that patients want. Two out of 3 consumers prefer to pay their medical bills electronically, and 56% are interested in or already using digital wallets such as Apple Pay and Google Pay for medical expenses.
Leveraging software-as-a-service solutions that provide digital communications and payment options enables providers to streamline billing workflows and drive cost efficiencies while enhancing patient engagement through personalized content and delivery channels. Better patient financial experience tracks directly to improved revenue cycle performance, including stronger cash flow and overall payments, and strengthens patient relationships to increase loyalty. This isn’t just about optimizing revenue; it’s about fostering a more sustainable and patient-centric healthcare ecosystem.
So many great answers here! Huge thank you to everyone who took the time out of their day to submit a quote! And thank you to all of you for taking the time out of your day to read this article! We could not do this without all of your support.
How do you think healthcare IT can help providers reduce denials and improve the success rate of claim reimbursements? Let us know over on social media, we’d love to hear from all of you!