Experian Health’s 2025 State of Patient Access: Key Findings & Trend
What You Should Know: – Experian Health today released its annual 2025 State of Patient Access Survey, revealing a healthcare landscape where patient perceptions of access have stabilized somewhat, yet significant disconnects remain between patient expectations and provider capabilities, particularly concerning digital tools and data accuracy. – While fewer patients report worsening access compared to ... Read More


What You Should Know:
– Experian Health today released its annual 2025 State of Patient Access Survey, revealing a healthcare landscape where patient perceptions of access have stabilized somewhat, yet significant disconnects remain between patient expectations and provider capabilities, particularly concerning digital tools and data accuracy.
– While fewer patients report worsening access compared to previous years, challenges persist in areas like scheduling speed, digital tool adoption, and front-end data collection, impacting both patient experience and provider operations.
Patient Access Perceptions: A Mixed Bag
The survey indicates a potential stabilization in access perceptions, with the highest percentages since 2022 reporting that access “was about the same” (68% of patients, 43% of providers). Fewer patients are reporting worsening access compared to prior survey years, potentially reflecting an overall better experience for some. However, a key friction point remains: among the 16% of patients who felt access improved, the top reason cited was the ability to see a practitioner quickly.
Conversely, for the 15% who felt access worsened, the primary challenge remained the difficulty in securing timely appointments. Compounding this, providers identified getting patients to actually use digital access services—often designed specifically to speed up scheduling—as their biggest challenge.
The Digital Divide: Scheduling Tools Wanted but Underutilized
There’s a clear patient demand for digital convenience, with 80% of those surveyed expressing a desire to schedule appointments anytime from their home or a mobile device. Despite this, providers are struggling to meet this expectation effectively. More than a third (37%) cited getting patients to use these digital tools as their top challenge, and over half (55%) believe patients are unsure how to navigate self-scheduling functionalities.
Providers recognize the need for improvement, with 71% calling enhancing the scheduling process an urgent priority. While adoption is progressing (54% currently offer self-scheduling and another 10% plan to within six months), persistent underlying issues continue to hinder access, including limited appointment availability (cited by 70% of providers), ongoing staffing shortages (63%), and long wait times (54%).
Data Accuracy Woes Impacting Care and Claims
Beyond scheduling difficulties, challenges with accurate data collection during registration and check-in create significant downstream problems for both patients and providers. The survey found that one in five patients face hurdles before even seeing a clinician due to data discrepancies: 22% reported experiencing care delays related to insurance verification issues, and 20% encountered errors in their medical records or billing information. Providers are feeling these strains operationally, with 56% stating that patient information errors are a primary driver of denied claims.
Furthermore, nearly half (48%) reported that data gathered during registration and check-in is often only somewhat accurate or not accurate at all. Adding to the complexity, while more patients report receiving cost estimates before care (41% in 2025, up from 29% in 2022), the perceived accuracy of these estimates has decreased (71% accurate in 2025, down from 78% in 2022).
Providers Prioritizing Accuracy and Automation for Front-End Processes
The survey also illustrates that providers have a strong awareness of these data integrity challenges and are prioritizing solutions. A significant majority see urgency in improving or implementing accurate cost estimates (88%) and deploying faster, more comprehensive insurance verification processes (83%). To address these critical needs, healthcare organizations are increasingly turning towards automation technologies designed to streamline front-end workflows.
“It’s great to see progress and a positive shift in how people feel about patient access, but there’s still more to do to make things smooth and clear for patients,” said Clarissa Riggins, Chief Product Officer at Experian Health. “That’s why Experian Health continues to focus on innovating to deliver solutions that meet evolving provider needs and improve the patient journey. Digital tools, patient portals and automation are just the tip of the iceberg as to what technology can do to modernize the healthcare experience.”
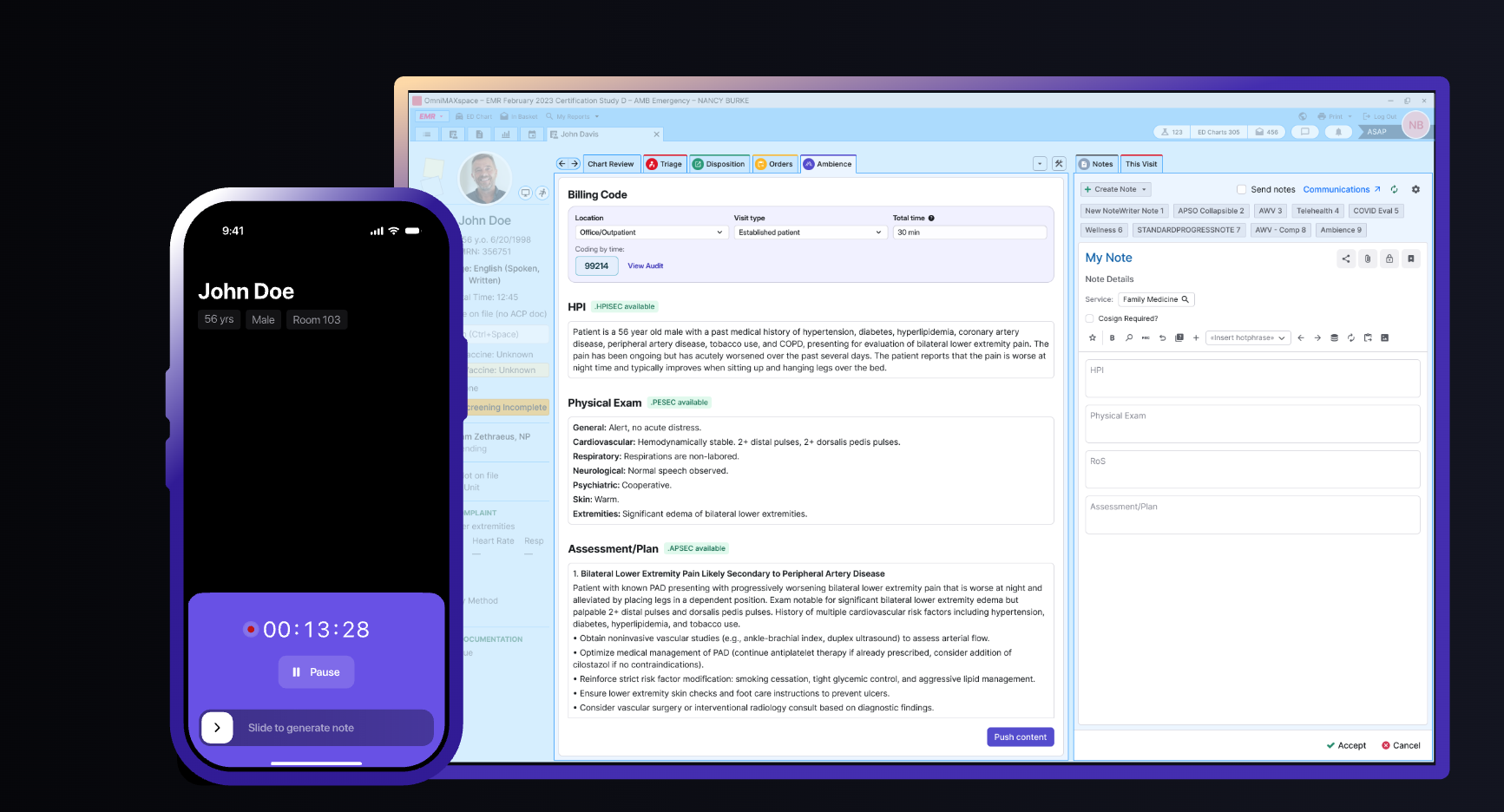
Solutions like Experian Health’s Patient Access Curator—which automates the real-time capture of critical patient information including eligibility verification, coordination of benefits (COB), Medicare beneficiary identifiers (MBI), insurance discovery, and demographics at registration—represent the type of tools being adopted to enhance data accuracy from the outset and improve overall efficiency.