With RCM Staff in Short Supply, Is AI the Missing Piece?
A hefty 63% of healthcare providers are grappling with revenue cycle management (RCM) staffing shortages, causing significant operational and patient-care challenges across the healthcare system. The staffing deficit has created a challenging cycle: understaffed RCM departments struggle to handle claims denials, leading to delayed reimbursements and increased administrative costs. When staff members spend excessive time ... Read More


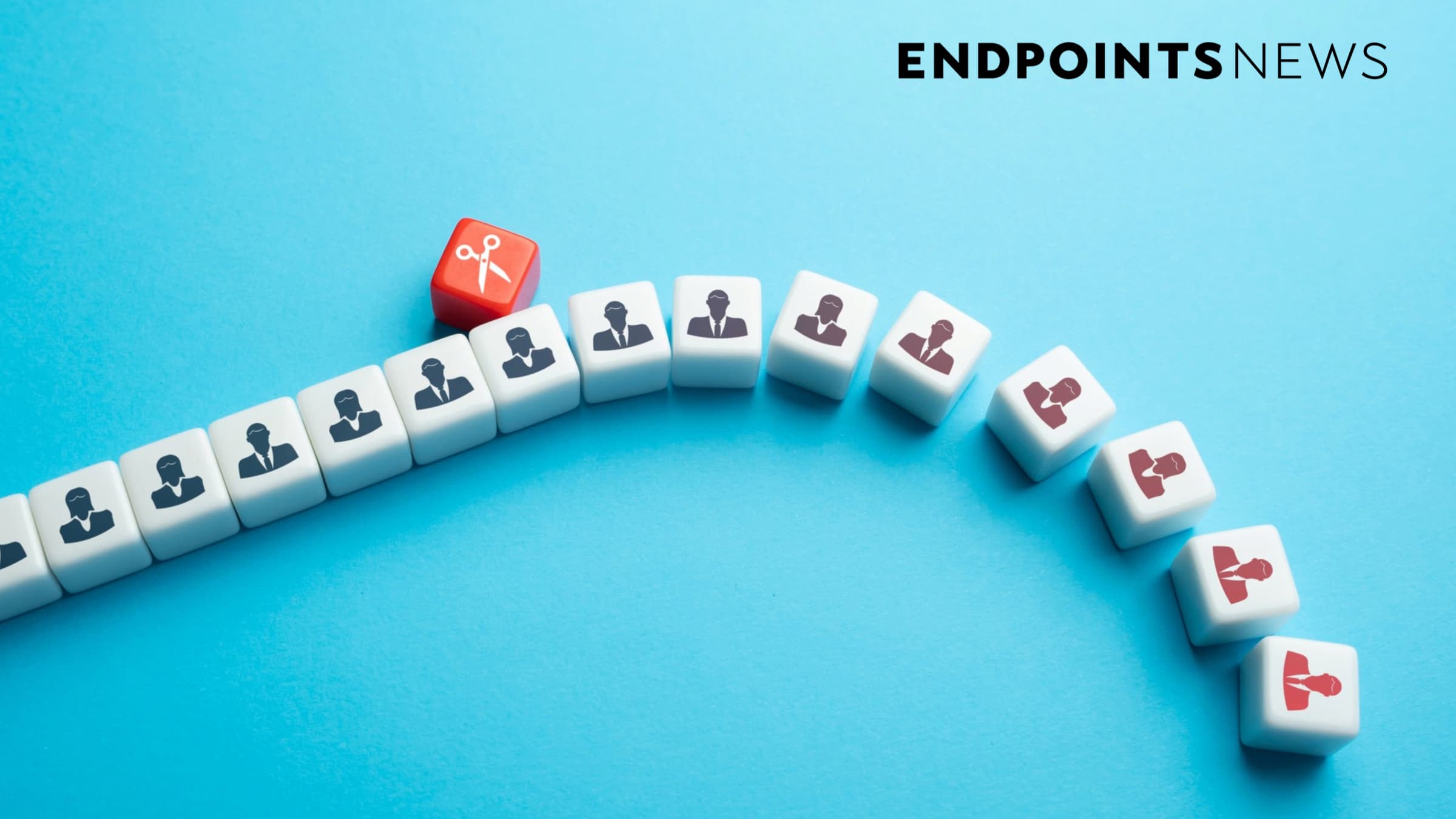
A hefty 63% of healthcare providers are grappling with revenue cycle management (RCM) staffing shortages, causing significant operational and patient-care challenges across the healthcare system.
The staffing deficit has created a challenging cycle: understaffed RCM departments struggle to handle claims denials, leading to delayed reimbursements and increased administrative costs. When staff members spend excessive time investigating and correcting denied claims, it prevents them from performing higher-value tasks and operating at the top of their license.
The impact reaches beyond administrative challenges into patient care. When claims are denied, patients may experience delays in receiving necessary treatments. Some might even avoid seeking care altogether due to financial concerns. A 2019 study published in the Journal of General Internal Medicine found that insurance claims denials were associated with decreased healthcare utilization and poorer health outcomes among chronically ill patients. This reality not only compromises patient health outcomes but also hinders the fundamental goal of physicians to deliver prompt and effective care.
Rising Solutions Through Technology
The scale of the current challenges has outgrown conventional revenue cycle management approaches. Artificial intelligence (AI) technology offers solutions that can reshape RCM operations, enabling healthcare providers to achieve new levels of accuracy and efficiency in response to advanced payer systems.
AI’s potential in revenue cycle management is multifaceted:
- Automation of repetitive tasks: AI can handle time-consuming, repetitive tasks associated with denials management. From data entry to claim status checks, AI-powered systems can process these tasks with greater speed and accuracy than human staff, freeing up valuable time for more complex activities.
- Predictive analytics: AI can analyze vast amounts of data to identify patterns and make predictions. In denials management, this means AI can predict which claims are likely to be denied before submission, allowing providers to address potential issues upfront.
- Intelligent appeals generation: When denials occur, AI can assist in generating accurate, compelling appeals. By analyzing successful appeals and understanding payer-specific requirements, AI systems can craft tailored appeals with a higher likelihood of success.
- Continuous learning and improvement: AI solutions learn and improve over time. As they process more data and encounter new scenarios, these systems become increasingly adept at managing denials.
AI Implementation Framework
From major hospitals to small practices, streamlining the revenue cycle has become essential as healthcare costs increase while reimbursements decrease. Rising denial rates across the industry compound administrative expenses.
While the potential of AI in denials management is clear, successful implementation requires a methodical approach. Consider these four essential components for effective AI-powered denials management:
- Well-defined use cases: Organizations must clearly define specific problems they aim to solve, whether reducing initial denials, improving appeal success rates, or identifying denials trends
- High-quality data: AI systems require comprehensive, accurate, and up-to-date data, including claims data, payer policies, clinical documentation, and historical denial patterns
- Automation platform: Successful AI implementation needs proper technological infrastructure for data ingestion, processing, and output, with capability to integrate with existing healthcare IT systems
- Skilled talent: While AI automates many tasks, human expertise remains essential. Success requires teams with combined skills in data science, healthcare domain knowledge, and change management
These four elements work together like components of a high-performance vehicle: the platform functions as the engine, data provides the fuel, use cases determine the track, and talent steers the course. Having sophisticated technology alone isn’t enough—success depends on how effectively these elements combine to deliver measurable results and genuine advancement.
The future of revenue cycle management
As healthcare costs rise and reimbursement rates decrease, improving revenue cycle efficiency has become essential for healthcare providers. AI offers a path to stabilize operations and increase revenue while allowing staff to operate at the top of their license.
For RCM professionals, AI serves as a supportive tool rather than a replacement. The technology helps staff by improving clinical data capture through analysis of unstructured data, automating the extraction of essential information from claims and medical records, and identifying emerging denials trends to prevent future issues.
When these pieces work together effectively, healthcare providers can better manage denials while maintaining financial stability in an increasingly challenging healthcare landscape.
About Spencer Allee
Spencer Allee is a data and AI leader with over 13 years of experience across multiple industries, including insurance, financial services, journalism, regulatory compliance, and healthcare. He has focused on building AI and ML platforms to accelerate knowledge work in complex business processes. Currently, Mr. Allee serves as Chief AI Officer at Aspirion, where he is building automation and data-driven intelligence into Aspirion’s RCM workflow to drive better outcomes for Aspirion’s clients.
Prior to Aspirion, Mr. Allee served as Chief AI Officer and Head of Product at Ascent RegTech, a cutting-edge regulatory compliance AI company that built a platform to automatically parse regulatory documents and rulebooks in the Financial Services industry. Prior to Ascent, Mr. Allee served as VP of AI & Data Solutions at Tribune Publishing Company.





































































































.jpg?#)






























