Using Real-World Data to Identify Barriers to Treatment Adoption
The following is a guest article by Noah Nasser, CEO at datma Understanding how and why new therapies are adopted—or not adopted—in real-world practice is critical to advancing precision medicine. While clinical trials may demonstrate efficacy, real-world adoption is shaped by far more complex factors, including diagnostic timing, provider behavior, and care coordination. Real-world data, […]

The following is a guest article by Noah Nasser, CEO at datma
Understanding how and why new therapies are adopted—or not adopted—in real-world practice is critical to advancing precision medicine. While clinical trials may demonstrate efficacy, real-world adoption is shaped by far more complex factors, including diagnostic timing, provider behavior, and care coordination. Real-world data, especially when structured into patient journey analyses, is emerging as a key tool for illuminating these patterns and identifying actionable barriers to treatment uptake.
Challenges in Treatment Uptake
Adoption is rarely uniform when new targeted therapies are introduced into routine clinical care. Despite strong clinical data, some therapies experience slower uptake across sites, regions, or patient groups. The therapies themselves don’t always drive these differences. Instead, they often reflect diagnostic workflows, coordination gaps, and physician decision-making. Delays in ordering or receiving test results, inconsistencies in how biomarker findings are acted upon, and breakdowns in communication can all limit access in ways that are difficult to detect without a more detailed view of how care is delivered.
From Discrete Events to Structured Patient Journeys
Many researchers and life science teams are turning to structured patient journeys to examine these dynamics more closely. These are time-sequenced snapshots of therapeutic and diagnostic events that allow analysts to trace a patient’s path from diagnosis through treatment. Rather than looking only at final outcomes or summary metrics, patient journeys help identify specific patterns in care, such as how long it takes to receive a test result, whether appropriate therapy follows, or where patients are lost.
These journeys are typically built from structured data extracted from systems like laboratory information platforms, pathology reports, and pharmacy records. Events are categorized by type, standardized, timestamped, and sorted to reflect the patient’s clinical experience over time. When organized properly, they make it easier to compare patients across sites or institutions and uncover variations in how care is delivered that might not be visible otherwise.
Diagnostic Context and Timing Matter
To fully understand how a therapy is adopted in practice, examining what happens before the treatment decision is important. This includes when diagnostic testing is ordered relative to diagnosis, whether results are returned in time to inform care, and how real-world prescribing aligns with expected treatment patterns. Delays in testing, slow turnaround of results, or inconsistencies in how physicians interpret results can all contribute to missed opportunities for treatment.
Any disruption between testing and treatment can significantly reduce uptake or exclude eligible patients for therapies that depend on biomarker identification. Structured patient journey data makes it possible to measure these sequences precisely and to determine whether care pathways support or hinder adoption. Without this level of visibility, it’s difficult to know whether challenges stem from knowledge gaps, workflow inefficiencies, or something else entirely.
Analyzing Patterns Without Centralizing Sensitive Data
The systems that store lab results, pathology findings, and imaging data are often siloed from traditional data warehouses. As a result, constructing patient journeys requires accessing and preparing data from multiple sources, each with its own privacy protocols and operational considerations.
To address this, some teams are applying federated approaches that allow patient journeys to be constructed and analyzed locally. Rather than sharing raw clinical data, institutions generate anonymized results on-site, enabling shared analysis without compromising governance. This reduces participation barriers and allows more diverse institutions to contribute, including those that might not otherwise engage due to privacy or resource concerns.
Applying These Insights to Market Access Strategy
For pharmaceutical companies seeking to improve market access and understand real-world adoption, visibility into diagnostic workflows and treatment handoffs can offer critical insights. Structured patient journey analysis provides a detailed view of when testing occurs, how long results take, and whether those results lead to appropriate treatment. These insights can help shape educational efforts, field strategy, and resource allocation, ensuring therapies reach the patients they intend to serve more efficiently and consistently.
They also help organizations assess how operational factors influence adoption, such as where delays tend to occur, which types of providers are slow to act on test results, or whether patients who test positive for a given biomarker are consistently receiving the associated therapy. By uncovering these patterns, teams can better understand how to bridge the gap between clinical intent and real-world implementation.
Toward a More Informed Approach to Adoption
As care becomes more complex and therapies more targeted, the ability to evaluate real-world care delivery is becoming essential. Structured patient journey analysis enables a deeper understanding of when and where adoption slows, and why. It allows teams to identify where patients fall through the cracks and where workflows must change.
When implemented thoughtfully, this approach supports a more complete, privacy-conscious approach of analyzing real-world data. It enables better planning, more effective engagements, and a clearer picture of how therapies are used outside clinical trials. For organizations focused on ensuring that innovative therapies reach the right patients, this level of insight is becoming an essential part of the strategy.
As pharmaceutical companies seek to accelerate adoption and reduce access disparities, structured patient journey analysis offers a robust, privacy-conscious way to pinpoint where the system is breaking down. Identifying specific bottlenecks in diagnostic workflows and treatment decisions empowers commercial, medical, and operational teams to develop more thoughtful strategies that reflect the realities of clinical care. In an era where precision medicine is only as effective as its delivery, understanding the full treatment journey is no longer optional—it’s essential.
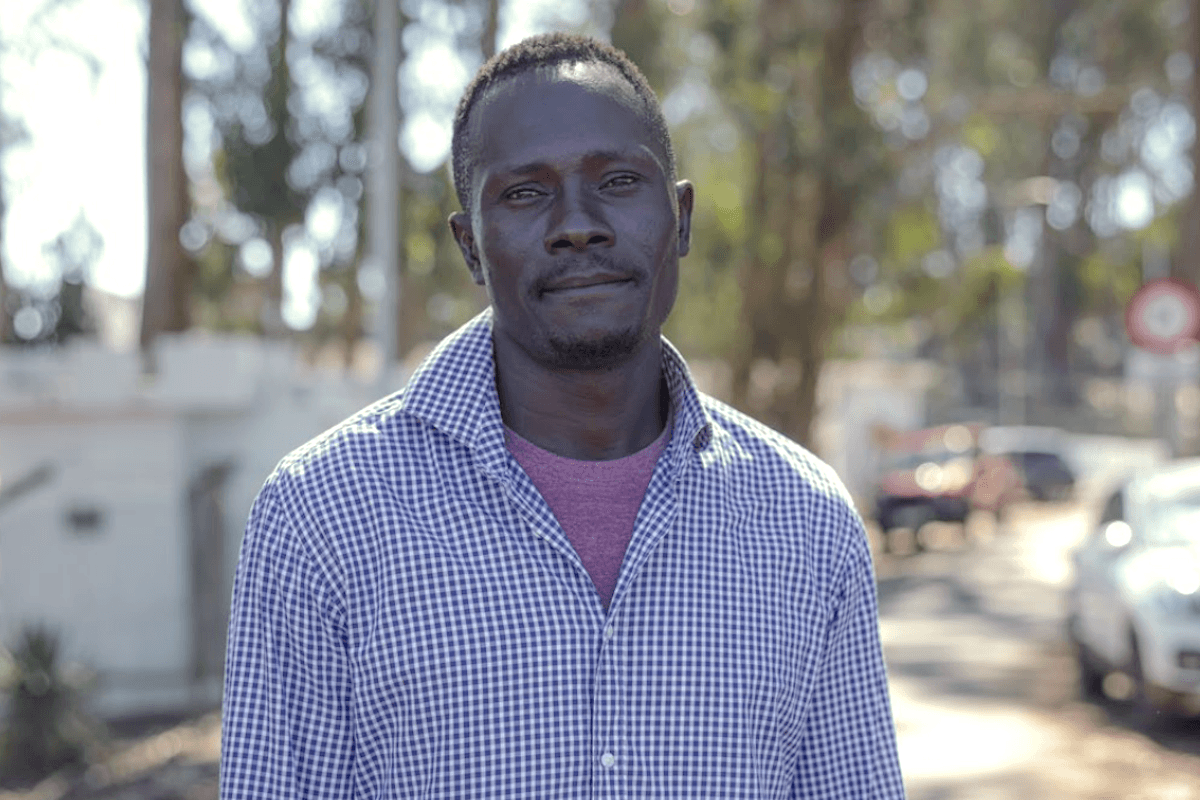
 About Noah Nasser
About Noah Nasser
Noah Nasser is the CEO at datma, a leading provider of federated Real-World Data platforms and related analytical tools. With more than twenty-five years of experience in biotechnology, Noah brings a broad background in developing and commercializing novel technology to advance human health, including serving as the CEO of Serimmune and Chief Commercial Officer roles at Human Longevity and Counsyl. Noah led Counsyl’s commercial team through its acquisition in 2018 by Myriad Genetics. He previously held senior leadership positions at AltheaDx and Verinata Health, a leader in non-invasive prenatal testing (NIPT), where he led his team through the company’s 2013 acquisition by Illumina. He holds a B.S. from the University of California, San Diego in Molecular Biology.