Q/A: Former HHS Commissioner on Why Medicaid is the Most Innovative Program in U.S. Healthcare
Medicaid plays a vital role in the American healthcare system, providing coverage for millions of vulnerable individuals. To gain a deeper understanding of the program’s evolving landscape, its unique strengths, and the challenges it faces, we spoke with Gary Jessee, Senior Vice President, National Consulting. With extensive experience on both the payer and provider sides, ... Read More


Medicaid plays a vital role in the American healthcare system, providing coverage for millions of vulnerable individuals. To gain a deeper understanding of the program’s evolving landscape, its unique strengths, and the challenges it faces, we spoke with Gary Jessee, Senior Vice President, National Consulting. With extensive experience on both the payer and provider sides, Jessee offers valuable insights into Medicaid’s role in addressing critical needs, from long-term services and supports to mental health care and social determinants of health. Our discussion explores how Medicaid is adapting to meet the changing needs of its beneficiaries and the broader healthcare environment, including the growing influence of technology and value-based care.
Can you provide specific examples of the unique services Medicaid covers that commercial payers typically don’t? What are the benefits and challenges of this broader coverage scope?
Gary Jessee, Senior Vice President, National Consulting: Absolutely. Medicaid provides many critical services that most commercial plans either do not cover or strictly limit as a benefit. The biggest is a category known as long-term services and supports or LTSS, which encompasses long-term stays in nursing facilities including room and board, personal care, and medical care. But it also covers residential care facilities for people with Substance Use Disorder (SUD), mental health disorders, and intellectual and developmental disorders. It can also include things like adult day care, non-emergency medical transportation, assistance with getting dressed or preparing meals or offering temporary respite for family caregivers. Medicaid is by far the largest payer of LTSS, followed by Medicare, with private insurers accounting for a much smaller sliver.
1. Additionally, for children and youth under 21, Medicaid’s Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) program ensures access to comprehensive preventive, diagnostic, and treatment services that go beyond the scope of most commercial plans.
2. Then there are the flexibilities granted to state Medicaid programs through the 1115 waiver program, which can expand eligibility and coverage for non-medical services provided by community-based organizations and nonprofits for projects that demonstrate alignment with the goals of the Medicaid program. Section 1115 waiver programs can provide assistance with housing vouchers for homeless individuals, nutritional assistance, or home modifications that enable individuals to remain independent.
3. These programs are especially vital for vulnerable populations, including seniors and individuals with disabilities, as they address both medical needs and social drivers of health. Research shows that when done well, these services improve quality of life for beneficiaries and lower overall healthcare costs.
How does Medicaid address the mental health needs of its beneficiaries? What are some of the key initiatives or programs that have shown success in improving mental health outcomes?
Gary Jessee: Medicaid is also the largest payer for mental health care in the United States. Over time, the program has evolved to embrace whole-person health as a more effective way to treat populations that often present very challenging combinations of behavioral and physical health conditions. Many states have embraced initiatives like Certified Community Behavioral Health Clinics (CCBHCs) and integrated physical and behavioral health services in the managed care contracts they award. For example, Texas found success using 1115 waivers to fund innovative approaches, including crisis intervention teams and expanded access to outpatient mental health services. The key is early intervention and ensuring mental health parity in benefits.
What is the role of Medicaid in providing housing assistance to its beneficiaries? How does stable housing contribute to overall health and well-being?
Gary Jessee: Stable housing is foundational to good health. For example, if someone has high blood pressure, is suffering from uncontrolled diabetes, has acute behavioral health issues and lives under a bridge, it’s going to be very difficult to engage that person in doctor’s visits. Medicaid promotes housing access by offering tenancy support services and partnering with housing authorities to fund supportive housing for individuals experiencing homelessness or managing chronic conditions. Programs that help people transition out of institutions into stable housing have resulted in documented improvements in people’s health status and cost savings.
How does Medicaid support the nutritional needs of its beneficiaries? Are there any specific challenges in ensuring access to nutritious food for Medicaid populations, and how are these being addressed?
Gary Jessee: Medicaid indirectly supports nutrition through programs like managed care initiatives that cover meal deliveries for post-hospital discharge programs or for high-risk populations. A few states use 1115 waivers to provide nutrition counseling, deliver prepared meals or provide prescriptions for fruits and vegetables. The challenge, of course, is that many Medicaid beneficiaries live in areas of the United States where they do not have access to healthy food. Partnering with food banks and community organizations is crucial in expanding reach.
What are 1115 waivers, and how are they being used to address significant healthcare challenges in 2025?
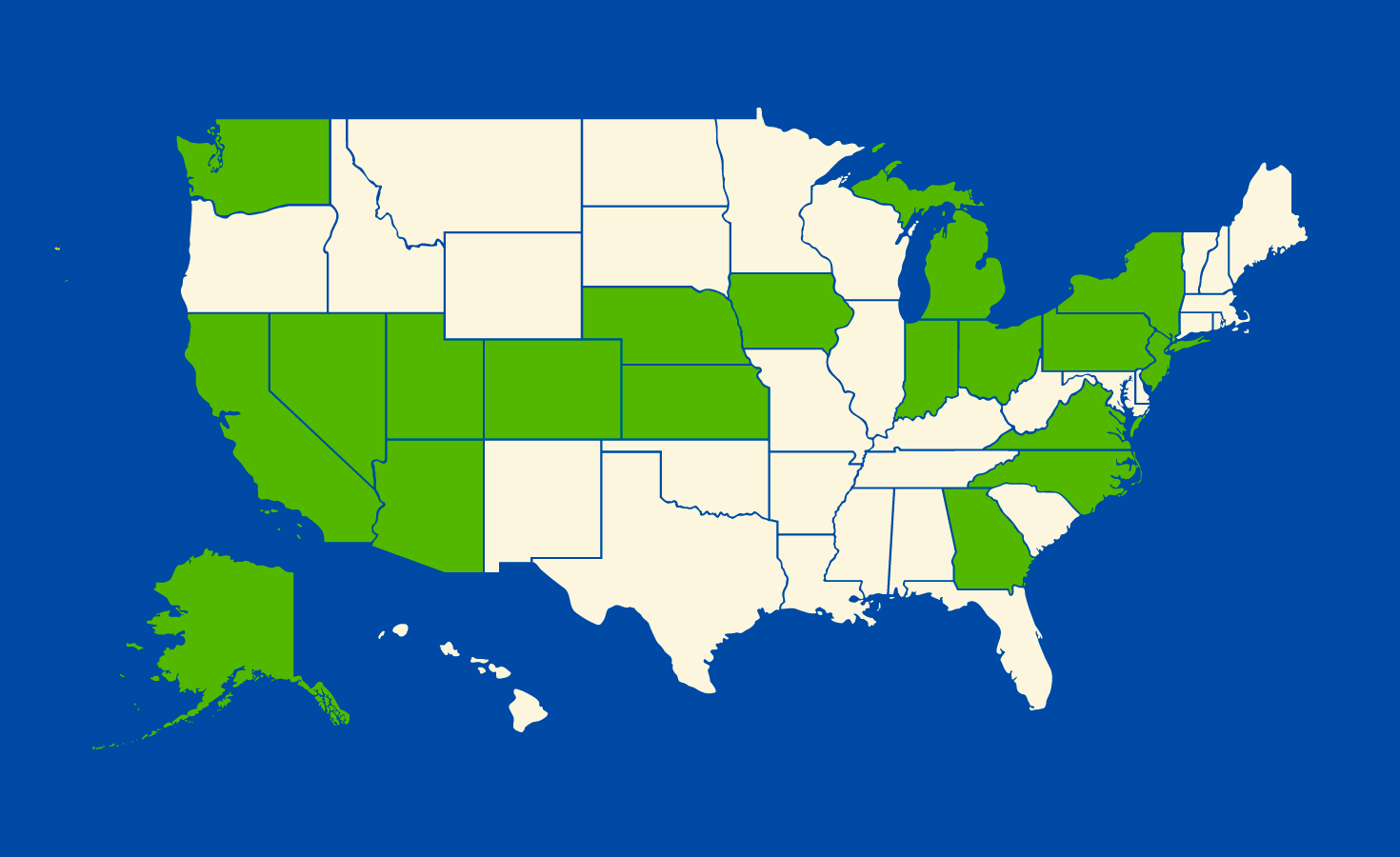
Gary Jessee: Section 1115 waivers allow states to pilot innovative programs to deliver and pay for Medicaid services. They’re critical for addressing pressing challenges like integrating care for behavioral and physical health, addressing social drivers of health, and improving maternal and child health outcomes. For example, last year CMS approved New York’s 1115 waiver to fund a three-year program to strengthen health equity and close disparities. The waiver is primarily intended to integrate physical health, behavioral health, and social care services, increase access to SUD treatment, invest in primary care, and shore up workforce shortages at safety net hospitals.
Based on your experience in Texas, what are some of the most innovative and impactful Medicaid initiatives you’ve observed?
Gary Jessee: Texas is a leader in innovative Medicaid programs, including its Delivery System Reform Incentive Payment (DSRIP) program under the 1115 waiver. This waiver encouraged providers to focus on outcomes and value-based care and was supported through a series of 20 regional healthcare partnerships to cover the entire state. Each partnership came up with its own plan for projects intended to reform how care was delivered. Additionally, initiatives to expand telehealth services for rural and underserved areas have proved to be game-changers, especially during and after the COVID-19 pandemic. These programs have not only expanded access to care but have also demonstrated cost-effectiveness.
Looking ahead, how will the Trump administration impact Medicaid policies and legislation?
Gary Jessee: It isn’t our place to make predictions, but we are closely monitoring developments. We are big supporters of fully funding Medicaid as a robust and innovative safety net healthcare program. If you cut Medicaid, you are hurting beneficiaries and also hospitals, which will face big increases in uncompensated care. Research has consistently shown that access to Medicaid coverage is tied to a host of health, educational and even economic benefits. I worked under governors throughout my career and in a state that did not expand Medicaid, and yet we still found ways to expand access under the program.
Lastly, how can Medicaid continue to evolve to serve its beneficiaries better and address the changing healthcare landscape?
Gary Jessee: Medicaid must embrace innovation and leverage data analytics to demonstrate its value in driving down costs and improving health outcomes. Integrating care, expanding telehealth, and focusing on social drivers of health like housing and food security are crucial. Collaboration between states, managed care organizations, and community partners will be key. Additionally, we need to maintain a focus on value-based care, ensuring resources are used efficiently while improving outcomes for beneficiaries.
And lastly, entrepreneurs are starting to see Medicaid in a new light. First, they’re realizing that Medicaid represents a vast, concentrated pool of individuals with similar health conditions, making it an incredible opportunity to target digital health solutions and create meaningful change. Second, despite the reputation for low reimbursement rates, many states utilize managed care organizations under risk-based contracts, offering untapped potential for innovation and impact to Medicaid.
About Gary Jessee, Senior Vice President, National Consulting at Sellers Dorsey
As the Senior Vice President of Sellers Dorsey’s National Medicaid Consulting Practice, Gary specializes in crafting and executing innovative solutions for a diverse clientele, including Medicaid agencies, managed care organizations (MCOs), private equity firms, child and family well-being agencies, and solution partners. Gary brings over 25 years of unmatched expertise in the Medicaid landscape with his background as a State Unit on Aging Director, state Medicaid director, and Deputy Executive Commissioner over all medical and social services. A highly recognized thought leader in the Medicaid landscape, he frequently speaks at national conferences on cutting-edge healthcare trends and best practices.































































.jpg)


































![[Industry Direct] Opening a New Chapter in VR Gaming – ‘The ChicKing Dead’ Enters Early Access!](https://roadtovrlive-5ea0.kxcdn.com/wp-content/uploads/2025/04/1_CKD_Main_Coverimage-341x220.jpg?#)





























