How Telemedicine is Revolutionizing Post-Acute Care for Faster Patient Recovery
The following is a guest article by Lesley Barton, National Clinical and Training Manager at Bunzl & AMHC As healthcare evolves, post-acute care has become a critical focus area, ensuring that patients continue their recovery outside of hospital settings. At the same time, telemedicine is transforming how post-acute care is delivered, by providing patients with […]

The following is a guest article by Lesley Barton, National Clinical and Training Manager at Bunzl & AMHC
As healthcare evolves, post-acute care has become a critical focus area, ensuring that patients continue their recovery outside of hospital settings. At the same time, telemedicine is transforming how post-acute care is delivered, by providing patients with faster, more accessible, and cost-effective treatment options.
The shift toward a connected health model, which emphasizes proactive, technology-driven care, is redefining patient recovery. With an aging population and a growing preference for home-based care, telemedicine is emerging as a key solution to help older adults manage chronic conditions while maintaining their independence.
As demand for quality, patient safety, and expanded care options increases, the healthcare industry is adapting with innovative telemedicine technologies designed to bridge gaps in post-acute care.
The Evolution of Post-Acute Care
For decades, post-acute care followed a straightforward discharge model: patients left the hospital with little follow-up, and their recovery largely depended on their own efforts. As one health system executive put it:
“In the old days, when we discharged patients from the hospital, you had this: ‘Goodbye and good luck. Nice knowing you. Hope everything is great. Drop us a postcard sometime.’ The future is that we are still responsible for that patient. Whether you own the facility, operate it, or not, you are now financially accountable.”
This shift in responsibility has redefined post-acute care, especially in response to new healthcare challenges and reimbursement models. Conditions that were once considered secondary concerns – such as pressure ulcers, incontinence, and post-surgical complications – are now being recognized as critical factors in recovery and quality of life.
Without proper post-acute care support, such conditions can significantly impact patient well-being, increase hospital readmissions, and complicate recovery. Addressing such challenges requires a proactive, long-term approach, so that patients receive the right support and the necessary resources to manage ongoing health concerns at home.
The Pandemic’s Impact on Post-Acute Care
A study found that during the height of the pandemic, post-acute care volumes declined significantly. Hospitals and care facilities were forced to cancel elective surgeries and reduce non-urgent admissions, following CDC recommendations to curb the virus’s spread. As a result, hospital revenue suffered, with facility utilization and healthcare spending dropping by nearly 40%.
Hospitals couldn’t afford any delays in finding a solution. The industry needed a way to continue post-acute care while ensuring patient and provider safety. This is where telemedicine took center stage, emerging as a critical tool to keep patients connected to their care teams without increasing their risk of exposure.
The Impact of Telemedicine in Patient Recovery
Telemedicine removes many traditional barriers to recovery, including:
Convenience and Accessibility
One of telemedicine’s most immediate benefits is convenience. Patients can consult healthcare providers from the comfort of their homes, eliminating travel time and reducing the burden of in-person visits. This is particularly valuable for individuals recovering from surgery or managing chronic conditions that make frequent clinic visits challenging.
Beyond convenience, telemedicine also breaks down geographical barriers. Patients in rural or underserved areas, as well as those who may have previously struggled to access specialized care, can now connect with medical professionals remotely.
Improving Care for Patients with Mobility Issues
For individuals with limited mobility or complex health conditions, telemedicine offers a lifeline to consistent care. Virtual consultations and remote monitoring allow patients to stay engaged with their treatment plans without the physical strain of travel. This is particularly beneficial for elderly patients and individuals with disabilities who may otherwise face significant challenges in attending in-person appointments.
Improving Continuity of Care
A coordinated approach to care is critical for post-acute recovery, and telemedicine strengthens communication between multiple healthcare providers involved in a patient’s treatment. Virtual platforms enable doctors, specialists, and rehabilitation teams to collaborate and care for all aspects of a patient’s health in real-time. This interdisciplinary model not only prevents gaps in treatment but also improves patient outcomes.
Helping Patients Reclaim Independence Through Virtual Rehabilitation
Early research defines telerehabilitation as “the application of telecommunication, remote sensing and operation technologies, and computing technologies to assist with the provision of medical rehabilitation services at a distance.”
The modern practice of telerehabilitation is removing traditional obstacles to care, making recovery more accessible, cost-effective, and personalized.
Beyond Traditional Rehabilitation: New Opportunities for Recovery
While the same source compared telerehabilitation to in-person therapy to determine whether it was “as good as” traditional methods, many experts now recognize that it offers distinct advantages. Virtual rehabilitation not only maintains the effectiveness of traditional therapy but expands access to patients who might otherwise go without necessary care.
Some of the key benefits of telerehabilitation include:
- Increased Accessibility: Patients in remote areas can connect with specialists without long-distance travel
- Flexible Treatment Plans: Remote sessions allow therapy to be integrated into daily life, making adherence easier
- Reduced Costs: Eliminating commuting, facility fees, and time off work makes rehabilitation more financially feasible
- Faster Intervention: Early detection of mobility issues through remote monitoring can prevent complications and reduce hospital readmissions
The Use of Innovative Devices in Virtual Rehabilitation
Advancements in technology are making remote rehabilitation both more interactive and effective. Several new smart devices, such as wearable sensors and remote assessments, have been developed to improve mobility and reduce the risk of falls, particularly for older adults and individuals recovering from injuries.
For instance, some devices detect improper use and transmit data to caregivers or medical providers, allowing for real-time feedback and training. Other devices analyze gait patterns to assess fall risk and provide insights into walking behavior improvements. Allowing therapists to adjust rehabilitation plans remotely.
Gamification and App-Based Recovery
Telerehabilitation is also integrating apps and gamification to make recovery more engaging and patient-driven. Mobile applications now offer:
- Personalized exercise programs customized to recovery goals
- Real-time feedback through motion-tracking technology
- Gamified rehabilitation exercises, where patients earn rewards or track progress through interactive challenges
- Direct access to therapists for remote check-ins, progress tracking, and virtual guidance
Wearable tech, interactive apps, and real-time monitoring all create a more dynamic and accessible recovery model that empowers patients to take control of their healing process.
Challenges in Expanding Virtual Healthcare (and How to Overcome Them)
While telemedicine has clearly transformed healthcare access and delivery, several challenges hinder its widespread adoption. From technological barriers to regulatory concerns, addressing these roadblocks is essential to keeping telemedicine a sustainable healthcare solution.
Bridging the Digital Divide
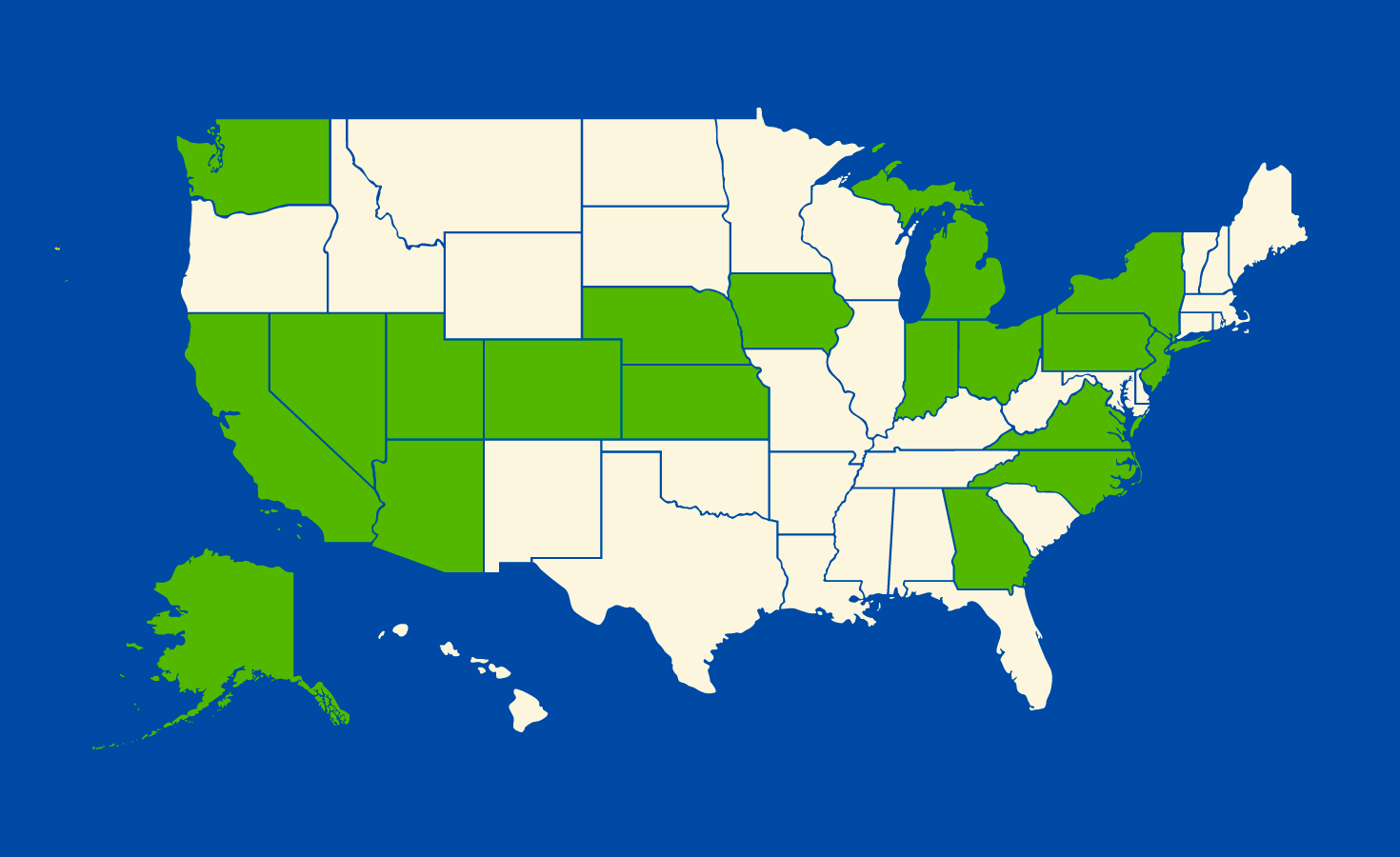
Disparities in digital literacy, technology access, and socioeconomic factors can create obstacles to telemedicine. Patients from vulnerable populations, including older adults, low-income communities, and rural areas, often struggle with virtual care due to a lack of reliable broadband services, limited access to smartphones or computers, and difficulty navigating telemedicine platforms.
To prevent telemedicine from widening healthcare disparities, policymakers and providers must focus on increasing accessibility. Digital literacy programs can help both patients and healthcare professionals gain confidence in using telehealth tools, while investments in broadband expansion can improve connectivity in underserved areas. Additionally, offering affordable or subsidized devices to those who need them can ensure that virtual care remains a viable option for everyone, rather than a privilege for the few.
Implementing Data Security and Regulatory Compliance
As telemedicine grows, patient privacy, data security, and compliance with healthcare regulations remain top concerns. Variability in telemedicine regulations across different regions adds another layer of complexity, making it challenging for healthcare providers to implement standardized solutions.
Key measures to address these challenges include:
- Developing clear telemedicine guidelines to ensure compliance with data protection laws (e.g., HIPAA, GDPR)
- Strengthening cybersecurity protocols to protect patient information from breaches
- Standardizing best practices for telemedicine providers to ensure consistent quality of care
Without solid security measures and regulatory frameworks, telemedicine services risk losing patient trust and facing legal roadblocks.
Integrating AI While Maintaining Human Oversight
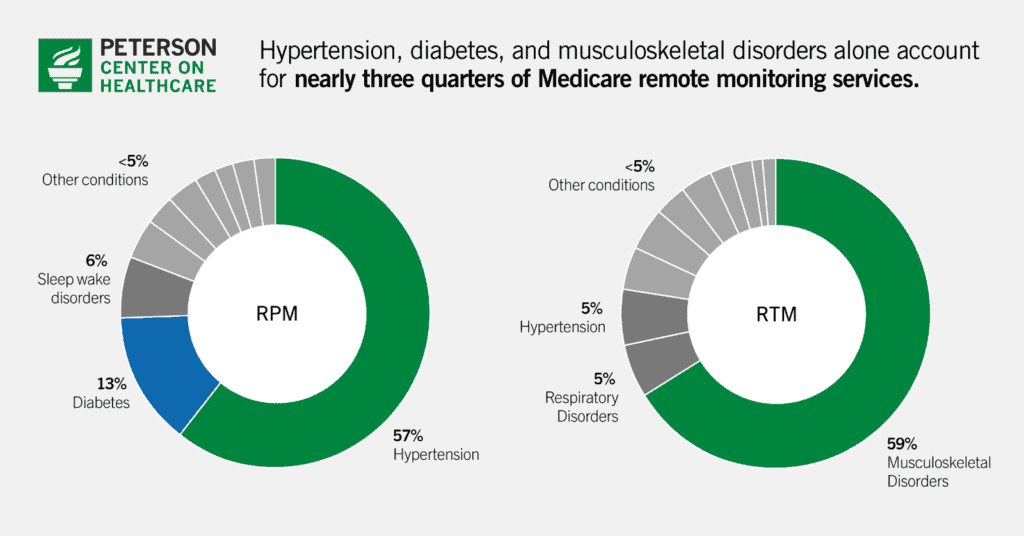
Artificial intelligence (AI) is becoming a key component of telemedicine, expanding its capabilities in several ways. For instance, remote patient monitoring helps track chronic conditions in real time, while automated diagnostic tools assist physicians in making informed decisions. AI is also reducing administrative burdens by streamlining paperwork and improving workflows.
However, physician oversight is still critical to maintaining accuracy, ethical standards, and patient safety. AI-driven tools should align with clinical practices, supporting (not replacing) medical expertise. Their design must prioritize usability and reliability, accounting for factors like reproducibility, availability, and cost.
Looking Ahead: A Telemedicine-First Future
According to McKinsey & Company, if telehealth adoption were extended equally across all patient populations, more than 50 million additional in-person visits per year could be converted to virtual consultations. This shift has the potential to reduce strain on healthcare facilities, allowing providers to allocate in-person resources where they are needed most.
As telemedicine continues to evolve, it is moving beyond a supplementary role and becoming a core component of post-acute care. Over the next three to five years, this shift will give patients greater flexibility in choosing between virtual and in-person visits, reshaping the way patients receive care, recover, and thrive.
 About Lesley Barton
About Lesley Barton
Lesley Barton’s extensive healthcare expertise and leadership have significantly contributed to clinical education and best practices. Her work with Bunzl & AMHC, alongside her role at the Continence Foundation of Australia, highlights her dedication to advancing patient care. Through the Clinical Care Connections (CCC) program, she has strengthened training initiatives in continence, wound care, and medical consumables. Lesley remains a key figure in shaping healthcare education and supporting clinical excellence across Australia.






























































.jpg)










































![The breaking news round-up: Decagear launches today, Pimax announces new headsets, and more! [APRIL FOOL’S]](https://i0.wp.com/skarredghost.com/wp-content/uploads/2025/03/lawk_glasses_handson.jpg?fit=1366%2C1025&ssl=1)

















