Microneedle patches could speed up diabetic wound healing
"The two approaches developed by our team would provide much-needed relief for patients with diabetic wounds..."

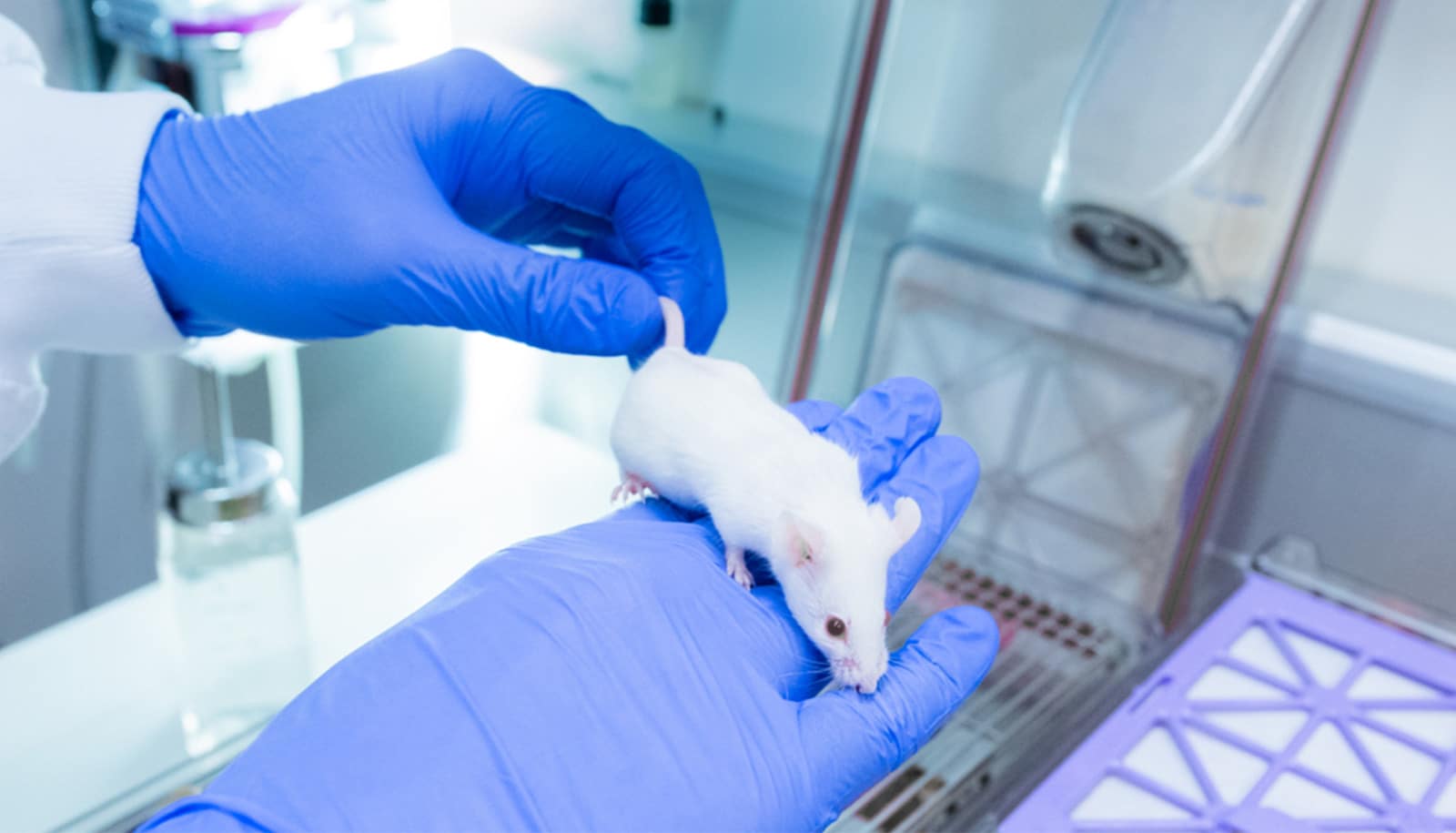
Researchers have developed microneedle technology to accelerate diabetic wound healing.
Diabetic wounds often lead to severe complications that can result in amputations. These chronic and non-healing wounds are marked by persistent inflammation, affecting more than 6% of the global population.
In Singapore, there are about four lower limb amputations daily due to non-healing diabetic wounds. A study focusing on diabetic wounds in Singapore estimated that the gross amputation-related healthcare cost per patient was S$23,000 (about $17,400 USD) in 2017.
To address this challenge of great national and global importance, researchers from the National University of Singapore (NUS) have developed two microneedle technologies that have shown efficacy in accelerating diabetic wound healing in preclinical models by preserving the functions of proteins called growth factors, and removing undesirable inflammatory compounds.
The two novel innovations were developed by a team of scientists led by Andy Tay, an assistant professor in the biomedical engineering department at the College of Design and Engineering at NUS and the Institute for Health Innovation and Technology.
“Growth factors are important for wound healing because they regulate key cellular functions. However, in diabetic wounds, these growth factors are rapidly broken down by other enzymes known as proteases. This dramatically slows down wound recovery. At the same time, diabetic wounds are characterised by persistently high levels of inflammation,” he explains.
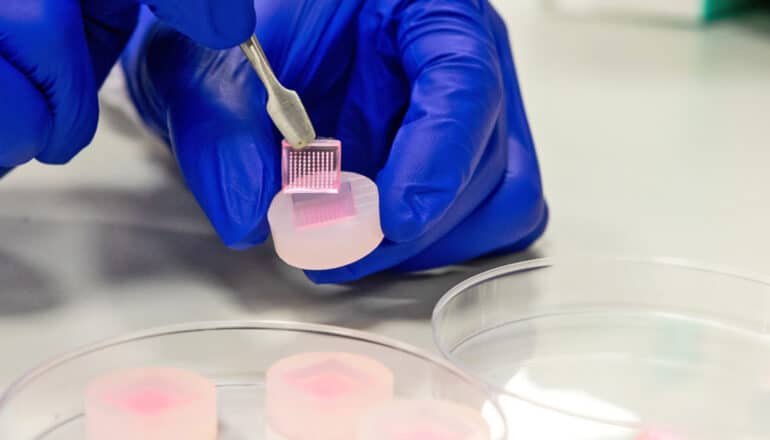
“We wanted to tackle these two issues by using microneedles for both delivery and extraction. It is minimally invasive, can be fabricated with precision, and allows for the active compounds to be painlessly administered directly into wounds. Microneedle patches are excellent materials for wound healing,” he says.
The results of the two related studies, which appear in the scientific journals Biomaterials and Advanced Functional Materials, demonstrate the potential of this innovative approach in treating various skin conditions such as psoriasis or chronic diabetic wounds.
2 unique approaches
In the market, hydrogel is used to deliver growth factors to wounds. However, this method is not as effective because the protease-rich environment of chronic wounds rapidly degrades and inactivates the growth factors. This means that the growth factors need to be delivered in high doses repeatedly, which can be costly and time-consuming.
In the first approach developed by the NUS research team, instead of delivering the growth factors directly, they first increased the production of growth factors within the wound.
They achieved this by developing sucralfate microneedles (SUC-MN) to deliver an important immunomodulatory protein, interleukin-4 (IL-4), to stimulate the production of growth factors in diabetic tissues. IL-4 helps to regulate the immune response and promote tissue regeneration, while sucralfate, a medication commonly used to treat gastrointestinal ulcers, protects growth factors from degradation.
The microneedles dissolve in the wound, delivering IL-4 and sucralfate directly to the wound. This localized delivery system minimizes systemic side effects, and also avoids secondary damage to delicate, newly formed tissues caused by traditional adhesive dressing that is currently used clinically. The researchers found that SUC-MN significantly accelerated wound healing twice as fast when compared to traditional treatments.
Although a majority of microneedle technology uses the material for delivery, the NUS team explored the novel use of microneedles to extract undesirable pro-inflammatory proteins and immune cells in the second approach. To do so, the NUS team needed to find a suitable coating material that could act as a sponge to soak up pro-inflammatory compounds, known as chemokines, which are “messenger” molecules that recruit and trap pro-inflammatory immune cells called monocytes in wound tissues.
The research team screened different materials and eventually used heparin-coated porous microneedles (HPMN) to address the issue of persistent inflammation in skin wounds at the source. Based on previous studies, heparin has been found to bind readily to chemokines. The team demonstrated that HPMN could effectively deplete chemokines and monocytes from the wound site, leading to a 50% reduction in tissue inflammation as well as a 90 per cent reduction in wound size by the 14th day of treatment.
These initial findings highlight the potential of HPMN as a promising strategy for the treatment of inflammatory skin disorders. The ability of HPMN to remove chemokines and inflammatory cells deep within the skin tissue offers a unique advantage over existing treatments that only target surface-level inflammation. HPMN could be further developed for personalized wound care and tailored treatment of various inflammatory skin conditions such as psoriasis.
Looking ahead
The development of SUC-MN and HPMN represents a significant step forward in the field of wound healing and skin disease management. The team intends to conduct further studies to explore the potential of this technology and bring it to market.
For extractive microneedles in particular, the team will fabricate microneedles with more controllable pore sizes using advanced technologies, such as 3D printing, and integrate antibacterial properties into the microneedles as clinical non-healing wounds often accompany infections. They are also designing flexible microneedle patches to ensure that they fit well to various tissue shapes.
“We are excited about the potential impact of our research and look forward to advancing this technology towards clinical translation. The two approaches developed by our team would provide much-needed relief for patients with diabetic wounds, as well as many patients suffering from skin conditions like atopic dermatitis or psoriasis,” says Tay.
Source: National University of Singapore
The post Microneedle patches could speed up diabetic wound healing appeared first on Futurity.












































































!['The Dream is [still] Alive': First IMAX film shot in space at 40 years](https://cdn.mos.cms.futurecdn.net/ii3bo2jM3f9hmrYbo3p7pF.jpg?#)
































![The breaking news round-up: Decagear launches today, Pimax announces new headsets, and more! [APRIL FOOL’S]](https://i0.wp.com/skarredghost.com/wp-content/uploads/2025/03/lawk_glasses_handson.jpg?fit=1366%2C1025&ssl=1)