Lena Health Raises $2M for AI-Powered Care Coordinator
What You Should Know: – Lena Health, an AI-powered care coordinator raises $2M in seed funding round co-led by Emergent Ventures and Cultivation Capital, the round saw participation from the Texas Medical Center (TMC) Venture Fund and Caravan Health Ventures (CHV). – The capital is designated for expanding the company’s services nationwide, enhancing its capabilities ... Read More
What You Should Know:
– Lena Health, an AI-powered care coordinator raises $2M in seed funding round co-led by Emergent Ventures and Cultivation Capital, the round saw participation from the Texas Medical Center (TMC) Venture Fund and Caravan Health Ventures (CHV).
– The capital is designated for expanding the company’s services nationwide, enhancing its capabilities for navigating complex community resource networks, and further augmenting care teams by automating routine, yet crucial, telephonic communication tasks.
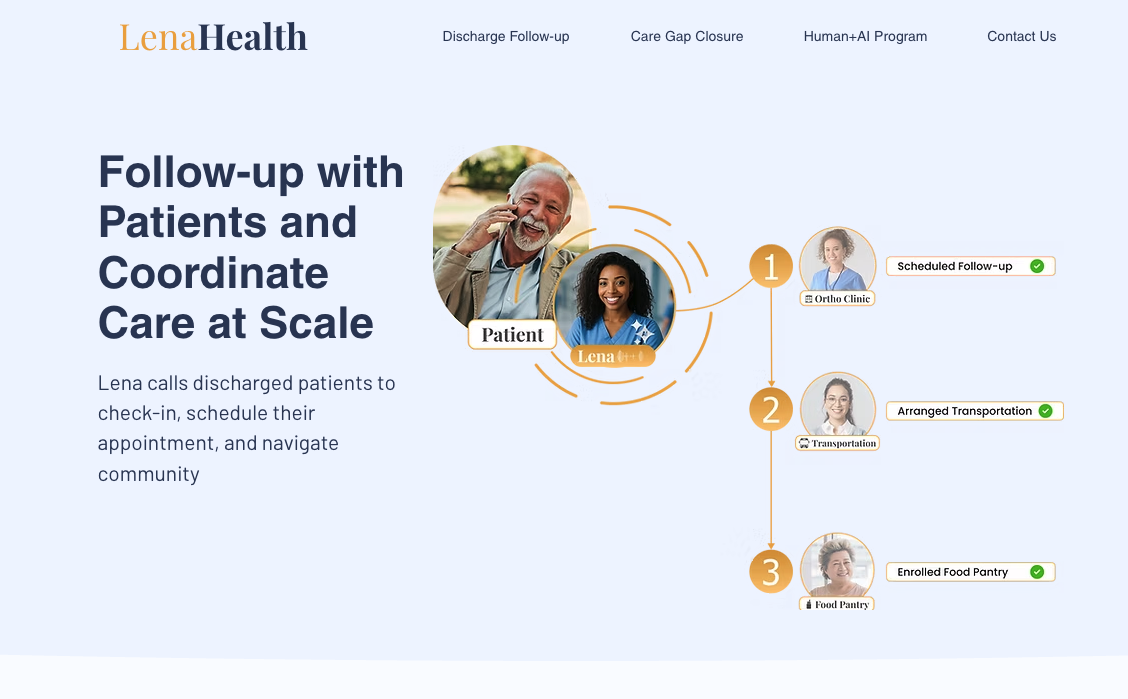
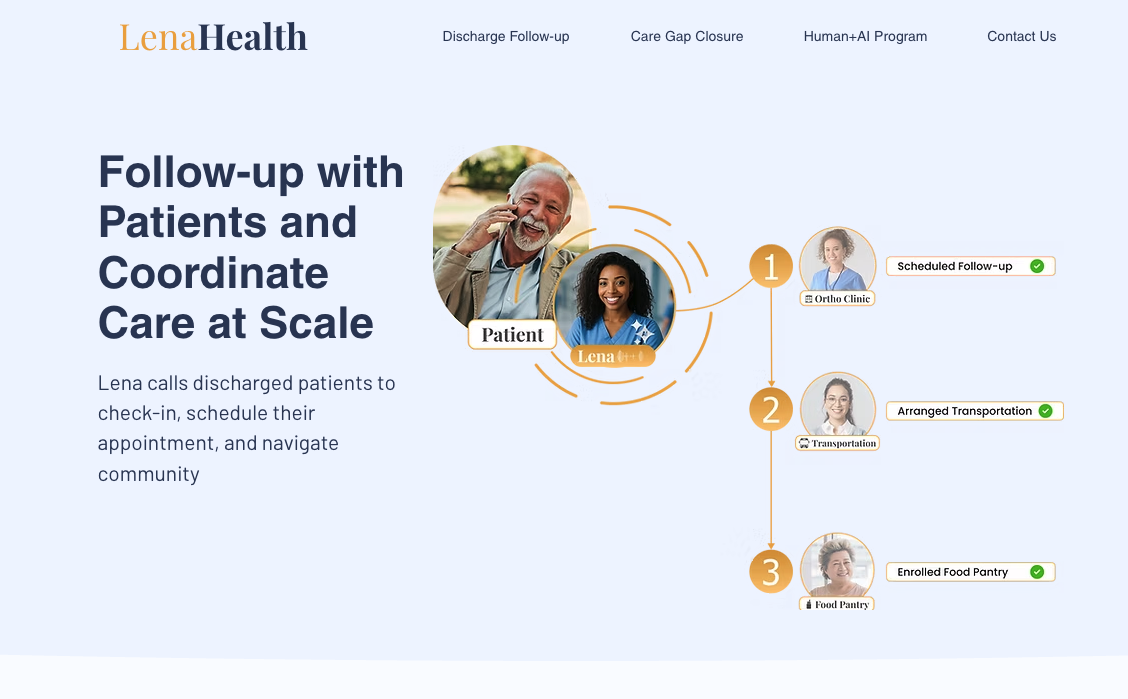
– Lena Health leverages artificial intelligence to proactively address patient clinical and social care needs, bridging gaps often missed in traditional care delivery.
AI-Powered Proactive Care Coordination
Lena Health’s core offering is an AI platform designed to anticipate and manage patient needs beyond the four walls of a clinic or hospital. It automatically handles critical tasks such as scheduling necessary follow-up appointments, coordinating medication management details, and connecting patients with vital community resources. This proactive approach aims to ensure patients receive continuous, comprehensive support throughout their care journey.
Delivering Value Across the Healthcare Ecosystem
The benefits of Lena Health’s platform extend to multiple stakeholders within the healthcare system. For Accountable Care Organizations (ACOs) and Clinically Integrated Networks (CINs), the AI coordinator drives improvements in quality metrics, increases opportunities for shared savings, and enhances the overall patient experience. Hospitals utilizing the system can expect reduced readmission rates, increased revenue from appropriate in-network appointments, and lower uncompensated care costs achieved by navigating uninsured patients to suitable primary care settings like federally qualified health centers (FQHCs).