Eliminating Cancer Treatment Side-Effects Through Targeted Drug Delivery
Last year, the American Cancer Society predicted that in 2024, the US would reach two million annual new cancer cases for the first time in history. This number is staggering and signifies that cancer is truly a disease that impacts many lives each day. While not all of these cases result in the grueling treatment ... Read More



Last year, the American Cancer Society predicted that in 2024, the US would reach two million annual new cancer cases for the first time in history. This number is staggering and signifies that cancer is truly a disease that impacts many lives each day.
While not all of these cases result in the grueling treatment associated with chemotherapy and radiation, many of those diagnosed will face the difficult road to recovery. Patients in chemotherapy experience a range of symptoms, from nausea to migraines and exhaustion.
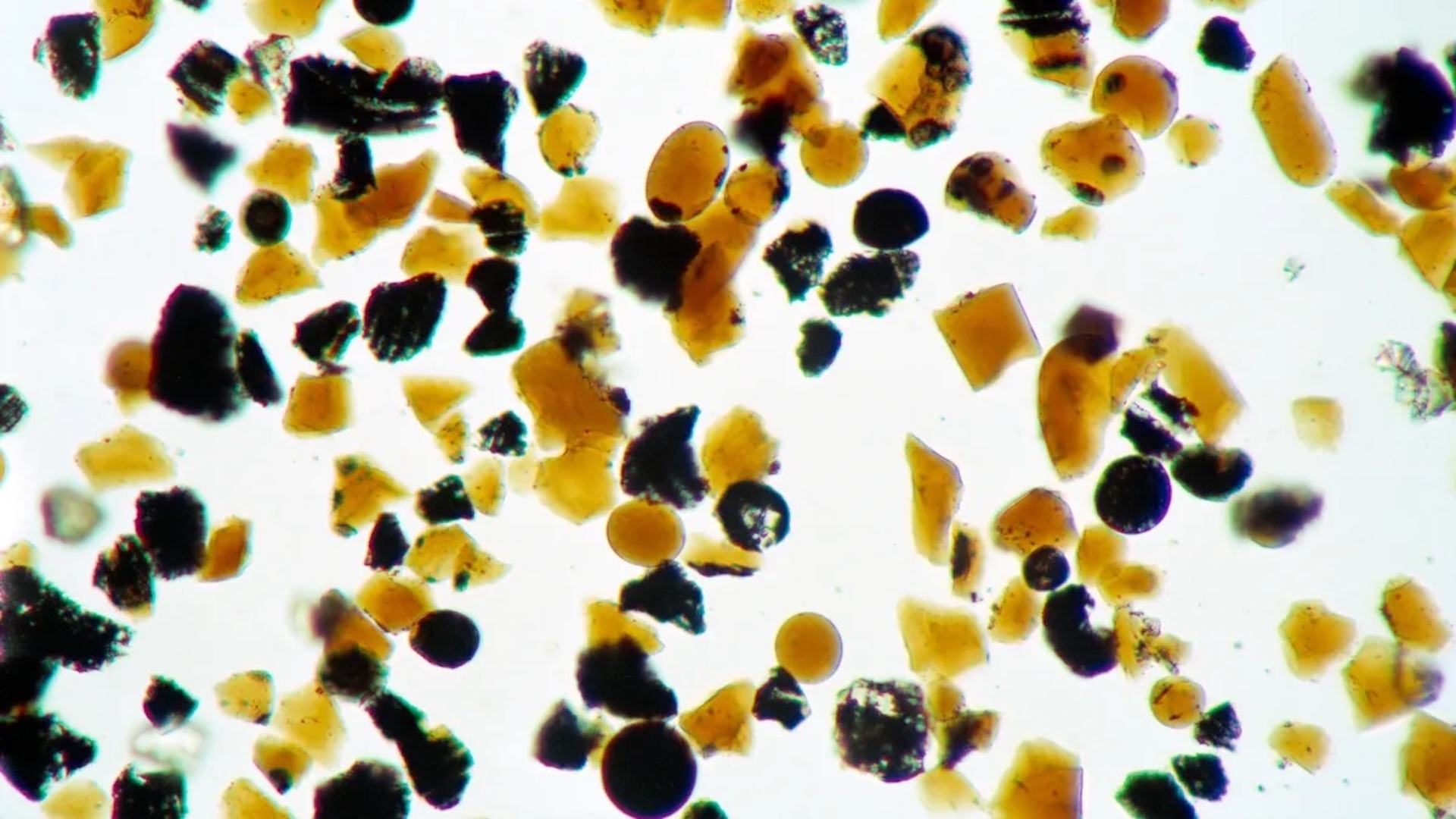
But imagine if there were a new course of treatment – one that could lessen side effects and improve the patient experience. Enter the radioligand, a microscopic particle containing a radioactive isotope and a cell-targeting compound called a ligand. The radioligand is injected intravenously, and a radiotracer ensures that the isotope targets the cancerous cells, boosting the potential to reduce cancer treatment side effects throughout a patient’s journey to remission.
Expanding the oncological toolkit
One in four people worldwide will develop cancer in their lifetime. Today, the go-to treatments are chemotherapy, radiotherapy, immunotherapy, and surgical procedures. Chemotherapy and radiotherapy aren’t targeted to specific cancerous cells, and therefore damage healthy tissues, causing life-impacting side effects. To address this, and spurred by new medical developments, a wave of new therapies is reshaping oncology. Immunotherapies, for example, stimulate the body’s immune system to help kill cancer cells. But there’s an even more precise way to fight the disease.
Targeted drug therapies increase the efficacy of cancer treatment, shorten recovery times, and help patients to live more independent lives. By lowering the amount of medication needed, targeted drugs protect healthy tissue and alleviate side effects. The benefits are myriad, supporting patients’ wellbeing while increasing their ability to stick with the treatment. One particular targeted therapy that has attracted heavy investment from pharma companies is radioligands. The market size of the radiopharma field is predicted to rise from $9.1 billion in 2023 to $26.5 billion in 2031 – a 14 percent compound annual growth rate.
Radioligands aren’t the only targeted drug delivery method. SonoTarg is working on an ultrasound-activated microbubble solution; the drug is encapsulated within the microbubbles and the ultrasound is pointed at the location of the tumor. When the drug passes the ultrasound, the bubbles burst and release the drug, the action of which is enhanced by the process. Separately, Pfizer has pioneered antibody-drug conjugates (ADCs) that combine antibodies and a cytotoxic drug to target and kill cancer cells. The first ADC was developed by Pfizer and approved by the Food and Drug Administration in 2000. Today, there are more than 100 ADCs used in clinical trials for numerous types of cancer.
Considerations such as updating care pathways and reimbursement models come with any new therapy. But for radioligands, the additional challenge is managing the radioactive elements to enable safe, accessible use. As the pace of medical development challenges the healthcare system’s ability to deliver, there’s a role for medtech and pharma companies to guide safe supply and embed radioligands into oncological treatment.
Put safety first
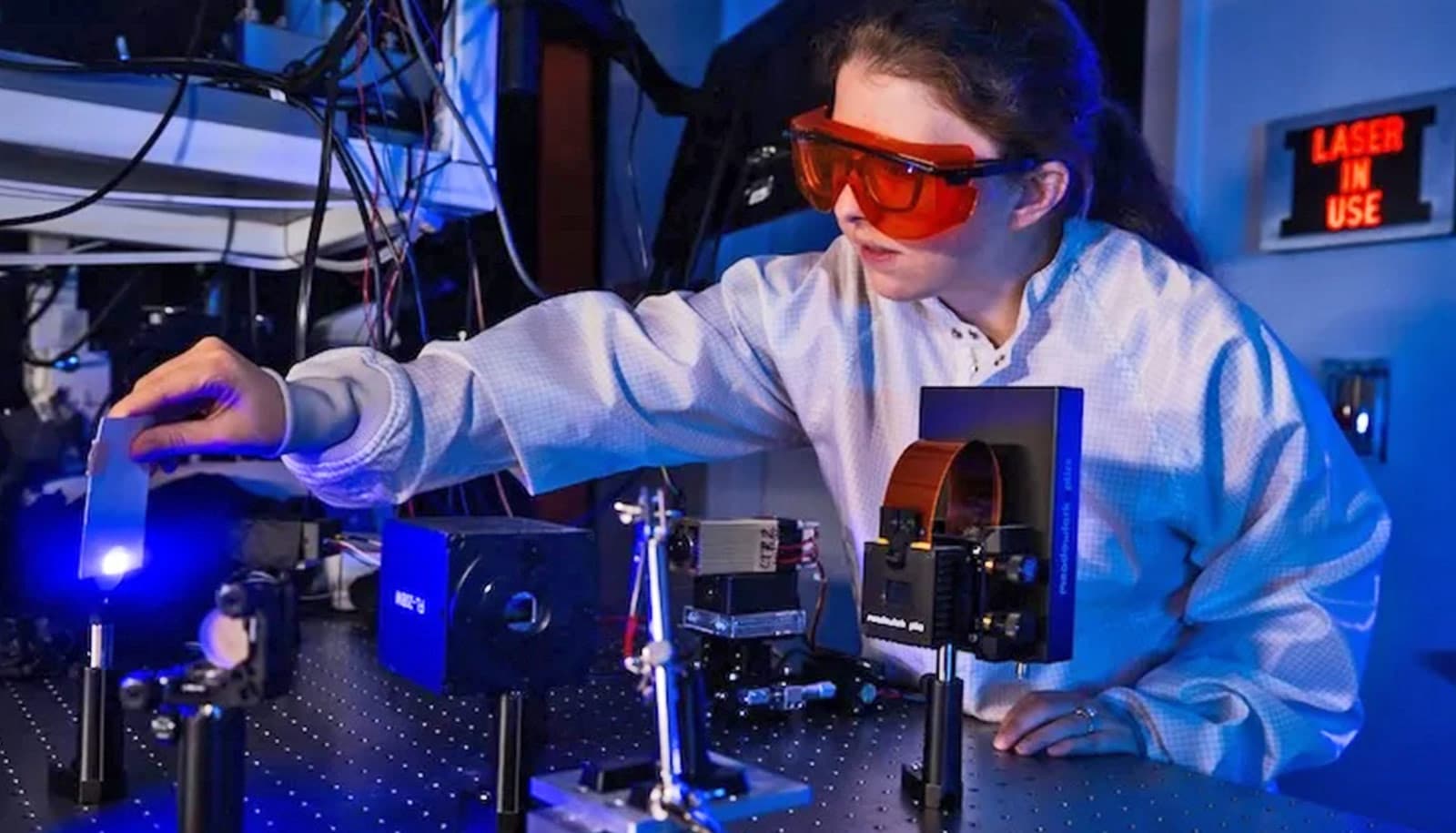
Due to a range of logistical and safety barriers, radioligands are limited in their reach. Success rests on overcoming not-insurmountable safety barriers. Perhaps the most complex step in expanding the use of radioligands is finding a better way to manage the radioactive properties. Areas with high potential for radioligand use (such as urology) aren’t necessarily equipped to handle radioactive substances, which complicates transport, delivery, and storage. The radioactive compounds are also in a constant state of decay and must be adjusted carefully to ensure patients receive the correct dose.
Currently, doses are calibrated using expensive, bulky equipment. Clinicians often need to modify doses based on patients’ biometric information, such as blood values. This calls for extensive safety training and the correct protective equipment. Further, radiation safety standards differ per location, necessitating contextual guidance on safe delivery and modification. There’s a sustainability angle, too – the containers that radioligands are shipped in aren’t currently reused or recycled, and reticence around waste materials has discouraged adoption.
Advice can be sought from other professionals, drug manufacturers, and medtech leaders. For example, a hospital is likely to have an existing radio-pharmacy and radio-oncology department, but few clinics are equipped with the necessary instruments, storage vessels, or on-site decay facilities to administer radioligands. A community urologist would need to upskill staff, update procedures, and perhaps change the layout of their clinic, which they could do more easily through partnerships. Similarly, if a clinic doesn’t have facilities to handle waste on-site, licensed waste management services can provide safe, off-site decay. Drawing on these wider resources shares risk while improving accessibility and trust.
Major on trust
For radioligands to work at scale, healthcare professionals need to trust the treatment, understand it, and be able to use it confidently. The human element – how clinical staff interact with emerging technology – is crucial. The clinical workflow will differ depending on the place of delivery, too, and the facilities that are available. Having the right workflows and assurances in place will help to create trust with all stakeholders, including but not limited to patients themselves.
The right training and socialization are central to ensuring that new techniques are prescribed and used in the best way, enhancing trust between partners in the ecosystem. This will make it much easier for clinicians to get it right, enabling them to trust in their own ability as well as the treatment itself. Medtech and pharma leaders have a role to play in providing, or at least informing, elements of training. Trust is equally important for those who are taking the drug. Patients need to trust that the therapy is safe and understand whether or not it will be covered by their health insurance.
Make it accessible
Pluvicto, a radioligand therapy for prostate cancer, is a single injection taken every six weeks that enables people to pursue their day-to-day activities after a two-day isolation period. Weighed against the ongoing side effects of conventional treatments, the isolation period is less disruptive to the patient’s lifestyle.
Democratizing access to radioligands and other targeted drugs relies on a distributed model supported by a network of partners. Pharma and medtech companies can partner with hospitals and clinics to co-develop new Standard Operating Procedures (SOPs) that align with hospital operations, clinical workflows, and preferred delivery methods, always with patient accessibility front of mind. Even if the treatment works and is trusted, extensive travel to hospitals or remote clinics can increase the likelihood of patient no-shows. If a patient can’t attend, not only do they fail to receive treatment, but a very expensive dose is wasted if the supply chain isn’t agile enough to repurpose it within the time window of effectiveness. While changing the model isn’t a small undertaking, the input of outside specialist radio-pharmacists, physicists, and contractors can smooth the process.
Accessibility is closely linked to the adoption of new payment models. In the traditional fee-for-service payment model, healthcare providers are reimbursed for the services they deliver. Profitability and revenue are driven by maximizing volume. Therapies such as radioligands buck the trend by reducing volume while delivering equivalent outcomes. This opens the opportunity for new alternative payment models (APMs) with payer organizations. Under APMs, healthcare providers are financially rewarded for saving on medical costs and delivering care more efficiently, incentivizing a switch from volume to outcomes-based models. Medtech and pharma companies can help providers to unlock these rewards by creating therapeutic solutions that improve the cost and quality of care. And this benefits all stakeholders, especially patients.
Maintain the pace of change through investment
Medical development tends to happen in smaller startup companies or academic research teams. Working hand-in-glove with a startup offers an opportunity for larger companies with shareholders to appease and targets to hit. Many companies are making significant financial commitments, too. Eli Lilly spent $1.4 billion on Point Biopharma, AstraZeneca snapped up Fusion Pharmaceuticals for $2.4 billion, and Bristol Myers Squibb paid $4.1 billion for RayzeBio.
And the investment is already beginning to pay off. Lutathera, a radioligand and radionuclide therapy, is treating patients with gastroenteropancreatic neuroendocrine tumors (GEP-NETs). Xofigo, another radioligand for prostate cancer but with a different mechanism of action than Pluvicto, is used to treat patients where other therapies are ineffective.
A world without cancer treatment side effects
In the next 10 years, radioligands could reduce side effects and improve recovery rates across a range of different cancers. When targeted oncological treatments such as radioligands are designed for individuals with unique conditions, as well as for diverse clinical teams, the more impactful they’ll be. One size certainly won’t fit all. By stepping into the role of partner and advisor, medtech and pharma organizations can help to build the all-important safety, accessibility, and trust that enables the healthcare system to meet people where they are.
About Bill Hartman
Bill Hartman is a pharma and medtech design expert at PA Consulting with over 25 years of experience across innovation strategy, new business development, and client programs in design research, strategy, and digital experiences.
About Tim Barrow-Williams
Tim Barrow-Williams is a professionally chartered engineer with extensive experience in medical device and drug-device combination product development. Tim leads PA’s work in drug delivery.