Addressing Challenges in Rural and Underserved Areas and Ensuring Equitable Access to Healthcare Services with Digital Health
While the world of healthcare has made a lot of exciting technologies and services to help improve the lives of patients and staff – there are always challenges in place that prevent people from accessing it. For example, telehealth allows people to have access to healthcare wherever they are, removing the barriers of location and […]

While the world of healthcare has made a lot of exciting technologies and services to help improve the lives of patients and staff – there are always challenges in place that prevent people from accessing it. For example, telehealth allows people to have access to healthcare wherever they are, removing the barriers of location and transportation. However, telehealth does require reliable internet access, which is not something readily available in rural and low-income areas. So in order for these services and technologies to function to their fullest potential, we need to address their challenges first.
To help discover these challenges and find some solutions for them, we reached out to our talented Healthcare IT Today Community to ask — How can digital health innovations address challenges in rural or underserved areas, ensuring equitable access to healthcare services?
Basia Coulter, Ph. D.d, Global Digital & AI Enablement Executive at Globant
Telemedicine has emerged as a particularly transformative tool, enabling rural patients to access specialists without long-distance travel, reducing wait times and emergency room overcrowding. However, barriers such as limited broadband access persist. Culturally tailored approaches are also vital – for example, designing interventions that align with local cultural norms, communication preferences, and trust dynamics. This requires a deep understanding of the values, traditions, and socioeconomic realities that shape health behaviors and access in rural communities.
AI-driven digital healthcare avatars, designed with multi-lingual conversational interfaces, could support post-discharge care by delivering personalized medication reminders and recovery guidance tailored to patients’ literacy levels and cultural and linguistic contexts. Integrating these avatars into existing telehealth platforms could enhance continuity of care, particularly in areas with clinician shortages, by providing 24/7 support for chronic disease management and adherence.
Matt Whitmer, Chief Revenue Officer at TeleVox/Mosaicx
Digital health innovations, such as telehealth services, AI chatbots, and virtual agents, are crucial in bridging the healthcare access gap in rural and underserved areas. These technologies enable patients to receive consultations, follow-up care, and health assessments without having to travel long distances. For example, mobile health apps can provide rural patients with self-management tools, and a live SMS chat allows them to connect with their provider regardless of time or location. By improving access to healthcare services and reducing logistical barriers, digital health platforms ensure that even those in remote areas can receive timely and effective care.
Dr. Lucienne Ide, Founder and CEO at Rimidi
Digital health innovations like remote patient monitoring (RPM) and chronic condition management (CCM) are transforming care delivery, particularly in rural and underserved areas where barriers to healthcare are common. Many patients struggle to receive necessary care or follow-ups due to transportation issues or inability to take time off work for in-person visits. RPM equips providers with valuable data from connected devices and patient-reported insights to bridge gaps in care, enabling proactive interventions and reducing the need for more frequent in-person appointments. These technologies are key to enhancing clinical efficiency and driving health equity so providers can deliver high-quality, patient-centered care regardless of geographic or socioeconomic barriers.
Lauren Barca, MHA, RN, BSN, VP of Quality at 86Borders
Digital health innovations have the power to transform care access in rural and underserved areas, but the real game-changer is how we use provider and plan member data. Remote monitoring tools – like smartwatches, condition monitors, and alert systems – offer a wealth of real-time health insights. The challenge isn’t just collecting this data. It’s ensuring it reaches the right hands at the right times. When care coordinators can act on accurate member data early, providers can intervene sooner, health plans can deploy resources faster, and ultimately, we can prevent costly ER visits and hospitalizations before they happen.
The biggest barrier in these member populations isn’t just geography; it’s data accuracy. The most vulnerable members often have the least documented health information, making timely interventions difficult. Health plans and providers must prioritize accurate member data and care coordination as a bridge between underserved populations and timely access to care. When we can locate and coordinate with every member, we will make healthcare more equitable.
David Harse, General Manager Patient Care at TruBridge
Everyone deserves access to quality healthcare, no matter where they live. Rural communities face mounting challenges, including provider and resource shortages, financial barriers, geographic distance, and broadband access. Technology is the most powerful lever to solve these problems. This is possible through collaborations with local providers who can help identify and solve challenges in their communities. Social determinants of health (SDOH) are critical factors that must not be overlooked as innovators identify and address care gaps. Additionally, industry consortiums such as the Trustworthy and Responsible AI Network (TRAIN) work to create unbiased frameworks for technology development. By working together, Health IT leaders can improve care delivery and create technology that drives equitable healthcare.
Dr. Javeed Siddiqui, Chief Medical Officer at TeleMed2U
Digital innovations like specialist telemedicine have the power to bridge critical healthcare gaps in rural and underserved communities, where access to high-quality medical care is often limited. Offering virtual consultations for a wide range of chronic conditions, ranging from diabetes to arthritis to mental health, enables patients to seamlessly connect with healthcare professionals without the need to travel long distances. This technology helps alleviate the burden of transportation costs and time, which can be especially challenging for individuals living in remote areas. It also allows for quicker follow-up care and condition monitoring longitudinally, ensuring that individuals can receive timely treatments and make necessary disease management interventions when they are needed, empowering users with timely clinical support that they might otherwise miss out on due to geographic isolation.
AJ Patel, CEO at TeleMed2U
While accessing specialist care can be challenging in urban areas, it’s even harder in rural communities. It is only by recognizing telemedicine’s true potential, which extends far beyond basic cough and cold diagnoses, that we can truly break down systematic specialist care accessibility barriers head on, harnessing the power of technology to make seamless patient connections to the high-quality care they need, when they need it. Over the past decade, specialist telemedicine has proven effective, overcoming geographical and logistical barriers quickly, connecting patients with the specialist providers they need, and creating a more equitable healthcare system for all. Leveraging the power of virtual platforms reduces the strain on local healthcare providers and improves health outcomes by ensuring that individuals receive comprehensive specialist care that addresses their specific needs and that they receive a proper diagnosis or treatment plan in a timely manner, putting them on a path towards better health longitudinally, regardless of where they reside
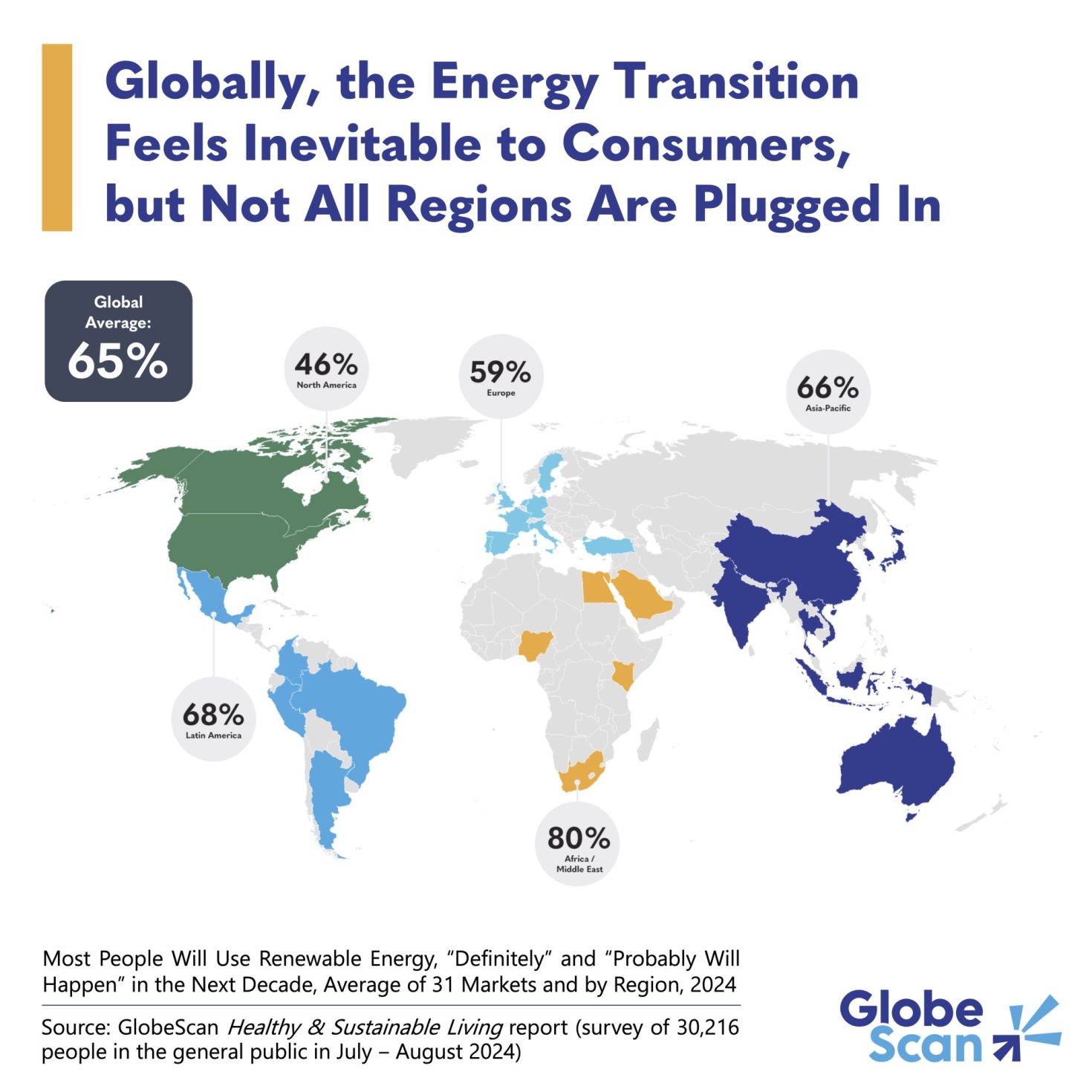
Brendan Smith-Elion, VP Product Management at Arcadia
Innovative digital health approaches—such as expanding specialized telemedicine applications, deploying healthcare AI chatbots, and leveraging digital community health worker solutions—can help bridge longstanding disparities in rural and underserved communities. Importantly, integrating social determinants of health (SDoH) and digital determinants (i.e., internet access, device availability, digital literacy) enables organizations to design targeted, effective interventions. For example, initiatives like the FCC-backed Connected Care Pilot Program implement community-based solutions that enhance broadband connectivity for rural populations.
At the same time, health systems have integrated proactive SDoH screening and virtual chronic care management for underserved communities. In addition, emerging programs to train local digital health navigators or community health workers in telehealth delivery technology have proven effective, helping patients navigate virtual care, improving health outcomes, and reducing gaps in care. By embedding equity metrics and incentives directly into risk-based contracts, healthcare organizations can further motivate targeted support and ensure sustained equitable access to healthcare innovations.
Jo Massoels, Chief Marketing Officer at Echosens
One of the biggest challenges in rural and underserved areas is limited access to preventive care and specialized services, leading to delayed diagnoses and poorer outcomes. Digital health innovations help bridge this gap by making critical screenings, diagnostics, and disease management more accessible. For conditions like liver disease, where early detection can make such a difference, cloud-based health platforms and portable, non-invasive diagnostic tools help providers identify at-risk patients sooner. By bringing innovative, scalable digital solutions into community health centers, mobile clinics, primary care clinics, etc., these healthcare organizations can help ensure geography doesn’t prevent patients from receiving care that previously may have only come from a specialist.
Jitesh Ghai, Chief Executive Officer at Hyland
As a tech CEO focused on data and emerging technologies such as agentic AI and genAI, I believe unstructured patient data presents a powerful opportunity to enhance healthcare access in rural and underserved communities. By harnessing the vast amounts of unstructured data in conjunction with AI capabilities, data such as physician notes, lab reports, patient surveys, and even audio or video inputs can be contextualized into information that enables more effective and equitable healthcare.
Agentic AI, for example, has the potential to change the way care is provided in rural or underserved areas by acting as a force multiplier for resource-strapped providers. Leveraging Agentic AI to reduce the administrative burden on healthcare organizations can free up additional resources to focus on providing higher levels of patient care and increasing the outcomes for the populations they serve. The ability to leverage AI and collaborate on medical images remotely represents a critical advancement in patient care, particularly for rural areas and time-sensitive conditions like strokes.
By enabling healthcare professionals to share and review high-quality diagnostic images in real-time, remote collaboration eliminates geographical barriers, ensuring rapid and accurate diagnosis. For patients in rural or underserved regions, this technology bridges the gap between them and specialized care, reducing delays that can be life-threatening in certain conditions. Ultimately, this approach enhances coordination across medical teams, improves patient outcomes, and fosters equitable access to high-quality healthcare.
Charlie Byrge, SVP Revenue at Tendo
Expanding access to care in rural and underserved areas requires affordable, transparent, and seamless healthcare solutions. Digital health innovations that offer nationwide networks of all-inclusive, bundled healthcare services with predictable pricing can help bridge these gaps. Platforms that enable patients to purchase procedures with upfront, transparent pricing—whether online or at the point of care—reduce financial uncertainty and improve access.
Additionally, direct contracting solutions that connect employers, care navigators, and TPAs with high-quality, bundled healthcare options ensure employees, regardless of location, can access cost-effective care. By streamlining access to predictable, affordable healthcare, these innovations help remove barriers and improve health outcomes for underserved populations.
What great insights! Huge thank you to everyone who took the time out of their day to submit a quote to us! And thank you to all of you for taking the time out of your day to read this article! We could not do this without all of your support.
How do you think digital health innovations can address challenges in rural or underserved areas, ensuring equitable access to healthcare services? Let us know over on social media, we’d love to hear from all of you!