Illuminated Smart-Lite Systems: A Simple Solution to Prevent IV Medication Errors
Ensuring patient safety in acute and critical care settings has become more challenging than ever before. Nurses, clinicians, and caregivers are facing more demands – often with fewer resources. They must juggle providing high-quality care while managing a growing number of patients, all under both physical and mental strain. In intensive care units (ICUs), where ... Read More


Ensuring patient safety in acute and critical care settings has become more challenging than ever before. Nurses, clinicians, and caregivers are facing more demands – often with fewer resources. They must juggle providing high-quality care while managing a growing number of patients, all under both physical and mental strain.
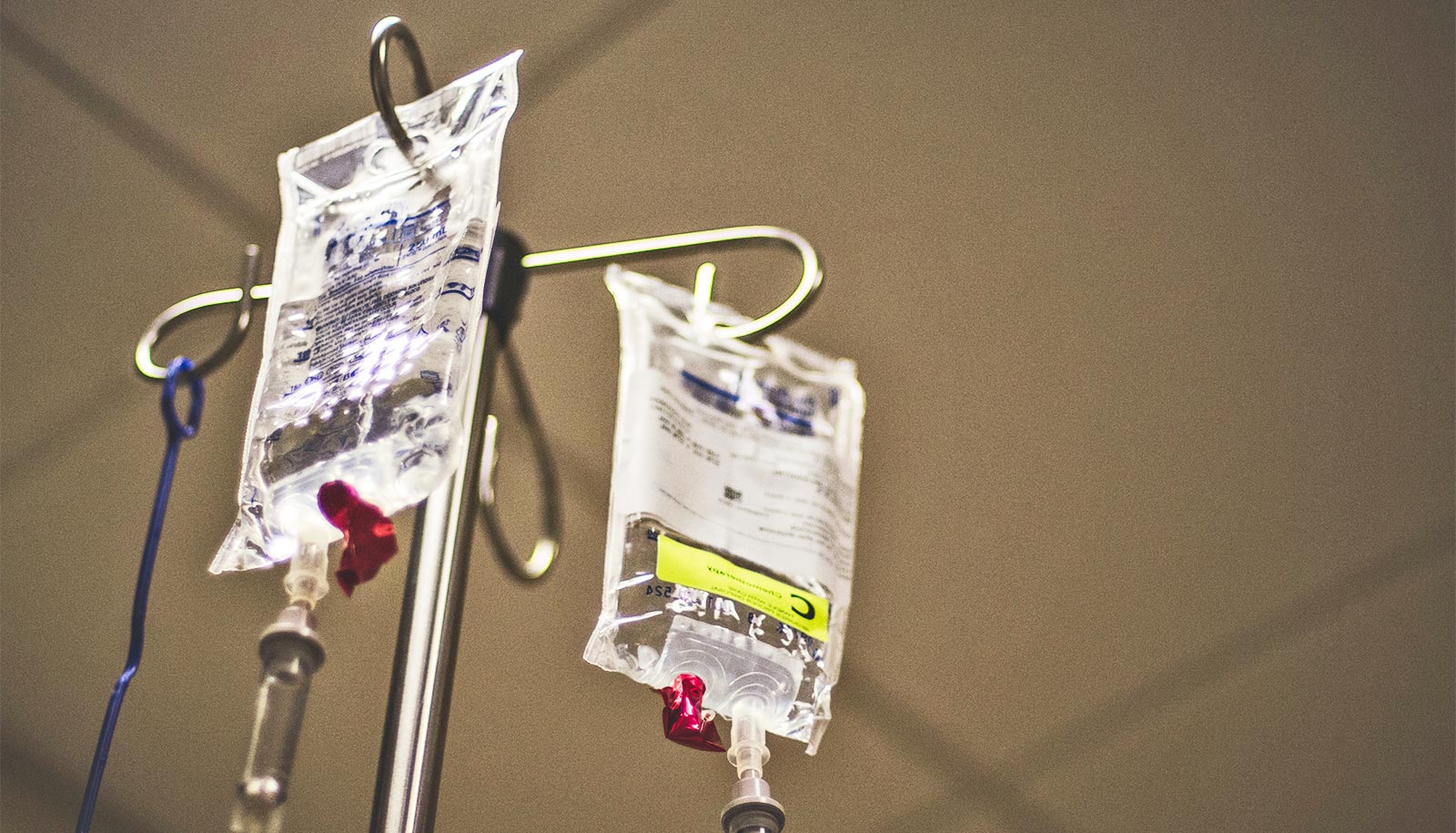
In intensive care units (ICUs), where nurses are responsible for managing multiple IV lines for each patient, labeling each line, and tracing each line – all compounded by shift change and patient transfer – the risk of serious medication errors is particularly high. Yet, despite the severity of the issue and requirements from the Infusion Nurses Society (INS), there is still no well-adopted method to quickly label and identify IV lines to prevent an ADE in most healthcare settings.
These challenges are compounded by serious post-Covid staffing shortages and the fact that ICU clinicians work in dim lighting, which makes it harder for nurses to properly trace IV lines. However, there is a simple and standardized solution that shows great promise – illuminated smart-lite systems. There is growing clinical evidence and use cases that demonstrate that this technology improves patient safety by reducing clinician mental tasks, speeding time to access the medication injection port, and reducing ADE errors.
The Scope of the Issue
Patient safety has always been a top concern in healthcare, and a 2016 study by Johns Hopkins highlights the scale and pervasiveness of medical errors. The study found that medical mistakes are the third leading cause of death in the United States, causing more than 250,000 deaths each year. Among these, infusion-related errors are a major issue, especially in critical care settings.
In 2022 alone, more than 1.25 million serious adverse drug events were reported worldwide, leading to nearly 175,000 deaths. One of the biggest problems contributing to these errors is known as “infusion confusion.” This happens when multiple IV lines get tangled up, making it difficult for nurses to figure out which one is which, facilitating a drug-to-drug ADE error potential. With ongoing staffing shortages and the pressure on healthcare staff increasing, we need solutions that can help reduce errors in all lighting conditions throughout the patient’s interdepartmental transition, while making the process of administering medications more efficient and safer.
Challenges in Acute and Critical Care Environments
In acute care settings such as ICUs, patients often need several IV lines to receive essential treatments like pain medications, antibiotics, and hydration. On average, an ICU patient in the United States has about eight IV lines, but in some cases, this number can climb to 15 or more. The more IV lines there are, the higher the risk of making a mistake. For example, a study from Kane-Gill found that for every extra IV line, the risk of a medication error increases by 3 percent, meaning a typical ICU patient has a 21 percent chance of experiencing an infusion-related error.
This issue is made worse by the ongoing nursing shortage, which only adds more stress to an already stretched healthcare system. During the “Great Attrition” in 2021 caused by the pandemic, up to 21 percent of nurses left the profession. Those who remain are expected to manage an even greater number of complex patient needs with fewer resources, making medication administration even more challenging. Nurses need tools that simplify their workflows and help them avoid making life-threatening errors.
In addition to the clear harm on patients and caregivers, medical errors have a significant impact on the bottom line. On average, healthcare providers are paying $450,000 in avoidable direct ADE costs per year per 100 beds in the hospital. This is from direct costs, and does not factor in labor, or patient harm liability suits. It is estimated that infusion-related errors are costing the U.S. healthcare industry up to $2 billion annually.
The Need for Standardized IV Line Identification
Despite the importance of IV infusion therapy, there is no universally effective standard in place to help identify lines clearly and quickly. Current methods to identify lines are time-consuming, lack standardization, and commonly involve the improvised use of labels and medical tape while not following the governing standards from the Infusion Nurses Society. Each line must be distinctly labeled, and the critical Keep Vein Open (KVO) line, which flows saline as a carrier for “as-needed” drugs, must be separate and distinctly labeled from all others (INS 8th Edition).
The current tape and label method is cumbersome for caregivers, making it difficult to apply labels to each line, repeat the process with line replacement routinely occurring per INS guidelines, and quickly distinguish and trace multiple infusion lines for every drug being administered. These lines often become easily tangled, leading to infusion confusion caused by what is commonly known as “spaghetti syndrome.” Shift changes, new or traveling nurses, and interdepartmental transport further contribute to the confusion. New pump systems, stacking the pumps vertically to save precious floor space, add a new complexity: the waterfall effect. In these vertically stacked pumps, the IV lines all exit in a “waterfall” on the same side of the stacked pump array, adding to the tangled line issue.
The size of the issue is alarming: 56 percent of all ADEs are infusion-related, with 15 percent of these being “wrong route errors” – the effect of caregivers injecting the correct drug, but choosing the wrong infusion line. Infusion-related ADEs can lead to severe patient harm and in the worst cases – even death. Addressing this issue is critical to improving patient safety.
Clinical Studies Validate Smart-lite Technologies
Another often-overlooked factor contributing to infusion mistakes is hospital lighting, or more specifically, the lack of it. Critical care units often use low lighting to help patients rest or per delirium protocols, but this can make it incredibly difficult for nurses to trace IV lines correctly. A peer-reviewed article published in the Journal of Infusion Nursing based on a study conducted at Wake Forest University School of Medicine found that nurses working in dimly lit ICUs took significantly longer to find the right IV line, further increasing their cognitive load and increasing the risk of a potential ADE.
Novel, yet simple, technologies such as illuminated smart-lite systems, could be a game changer in reducing infusion confusion. These technologies use illuminated guidance systems to visually identify each IV line. This simple yet effective solution makes it much easier for nurses to identify the correct line, accelerate access to the drug delivery port, and administer drugs without error.
The Wake Forest University School of Medicine clinical study demonstrated that nurses using illuminated smart-lite technology were able to locate the primary medication line 24 percent faster than those using traditional labeling methods, also reporting a 40 percent reduction in quantified cognitive load while having zero errors in darkened room conditions common in the ICU. This technology not only improves visibility but also reduces the mental strain on nurses, ultimately leading to fewer mistakes and better patient outcomes. Importantly, the solution attaches to any common standard-diameter IV line today, can be disposed of in standard waste, lasts for 96 hours tied to common INS guidelines for line-change protocols, and can be deployed hospital-wide in less than one half-day of in-service.
The effectiveness of illuminated smart-lite systems was also validated by a four-month study conducted at a major U.S. Veterans Affair (VA) Hospital in Houston, Texas within the MICU, SICU, and ICU. The research tested the level of improvement in the time to access a patient’s medication port. Normalized for the number of lines per patient, illuminated smart-lite systems improved the time of injection readiness by over 400 percent. Additionally, the traditional standard of care took between 19 to 58 seconds to reach the port as compared to smart-lite systems, which only took 1 to 7 seconds.
Combined with the ability to use these in all lighting conditions, which creates a simplified method to meet the required mandate by the INS for line identification, smart-lite systems bring a necessary simplicity to a messy situation.
Prioritizing Patient Safety Through Innovation
Infusion-related errors are still a major problem that healthcare providers cannot afford to ignore. Preventable patient harm associated costs to the hospital and liability are all widely understood to this unchecked sentinel patient harm event. As patient needs become more complex and staffing shortages continue, it is crucial that healthcare systems invest in solutions that improve efficiency, standardization, and safety in IV therapy; all while being nurse-championed as powerfully simple to adopt.
Illuminated smart-lite technologies provide a simple but powerful way to reduce wrong-route infusion errors and protect both patients and healthcare staff. By improving visibility and streamlining workflows, these technologies help prevent mistakes and, most importantly, save lives.
By shining a light on infusion safety – both literally and figuratively – hospitals and healthcare organizations across the globe can take proactive steps to reduce errors and create a safer, more efficient care environment.
About Rodney W. Schutt
Rodney W. Schutt is the President & CEO of Orion Innovations, a healthcare technology platform company advancing smart, simple, and patented solutions that improve patient safety and enhance the bottom line. This includes the MedLite ID solution, which is an nine-time patented smart-lite product designed to simplify the current line-tracing process in acute care settings and reduce the chance of IV infusion-related errors leading to a wrong-route Adverse Drug Event (ADE).