How 3D Modeling is Transforming Medical Imaging and Diagnosis
In the 21st century, we are fortunate to benefit from perpetual advances in medicine. Researchers continue to discover new procedures and treatments, and those advances often rely on technology. Improvements in hardware, internet speeds, interconnected devices, and artificial intelligence all contribute to higher efficiency, personalization, and accessibility in treatments. Technologies such as advanced imaging and ... Read More


In the 21st century, we are fortunate to benefit from perpetual advances in medicine. Researchers continue to discover new procedures and treatments, and those advances often rely on technology. Improvements in hardware, internet speeds, interconnected devices, and artificial intelligence all contribute to higher efficiency, personalization, and accessibility in treatments.
Technologies such as advanced imaging and modeling (AIM), augmented reality/virtual reality (AR/VR), 3D printers, AI, and hardware integrations are dramatically impacting diagnosis, surgical procedures, and individualized treatment. The ability to create dynamic three-dimensional models and realistic environments has revolutionized medicine, including doctor training, surgical planning, prosthesis design, and patient education. Here are just a few examples of 3D development’s impact on the medical space:
- At Johns Hopkins, neurosurgeons use AR headsets to view 3D images of the patient’s brain, reducing surgical planning by 25% and improving tumor resection accuracy by 10%.
- The Norwegian University of Science and Technology (NTNU) have developed a way to create a 3D image of a patient’s colon from a single endoscopy image, making disease diagnosis faster and more accurate.
- Case Western Reserve University uses HoloAnatomy software with AR headsets to teach anatomy, improving test scores by 40% and reducing time to master anatomical concepts by 35%.
- Unlimited Tomorrow is using Siemens Xcelerator software to design custom prosthetic arms for Ukrainian soldiers.
Custom software development and integration with other technologies are proving invaluable for improving healthcare. Here are a few areas where custom 3D development is especially successful.
Surgical Planning and Simulation
The ability to model complex anatomy and create anatomical models specific to a patient’s needs makes surgery faster and more precise. Drawing from medical imaging data, such as CT and MRI scans, detailed models can guide preoperative planning and support surgical simulation.
3D models are especially useful for orthopedic and reconstructive surgery. Surgeons can use the models to accurately simulate the correction of deformities before starting the procedure. Medical models must be accurate and precise. The more personalized the models, the more valuable the images are for surgical planning and simulation.
For example, Arthrex has developed VIP, preoperative planning software that helps surgeons and patients. VIP helps surgeons size and optimize shoulder arthroplasty implants and quickly develop a comprehensive, patient-specific, preoperative surgical plan. The software integrates with MyVIP, an app that helps explain the procedure to patients, providing presurgical information to tell them what to expect from their implant surgery.
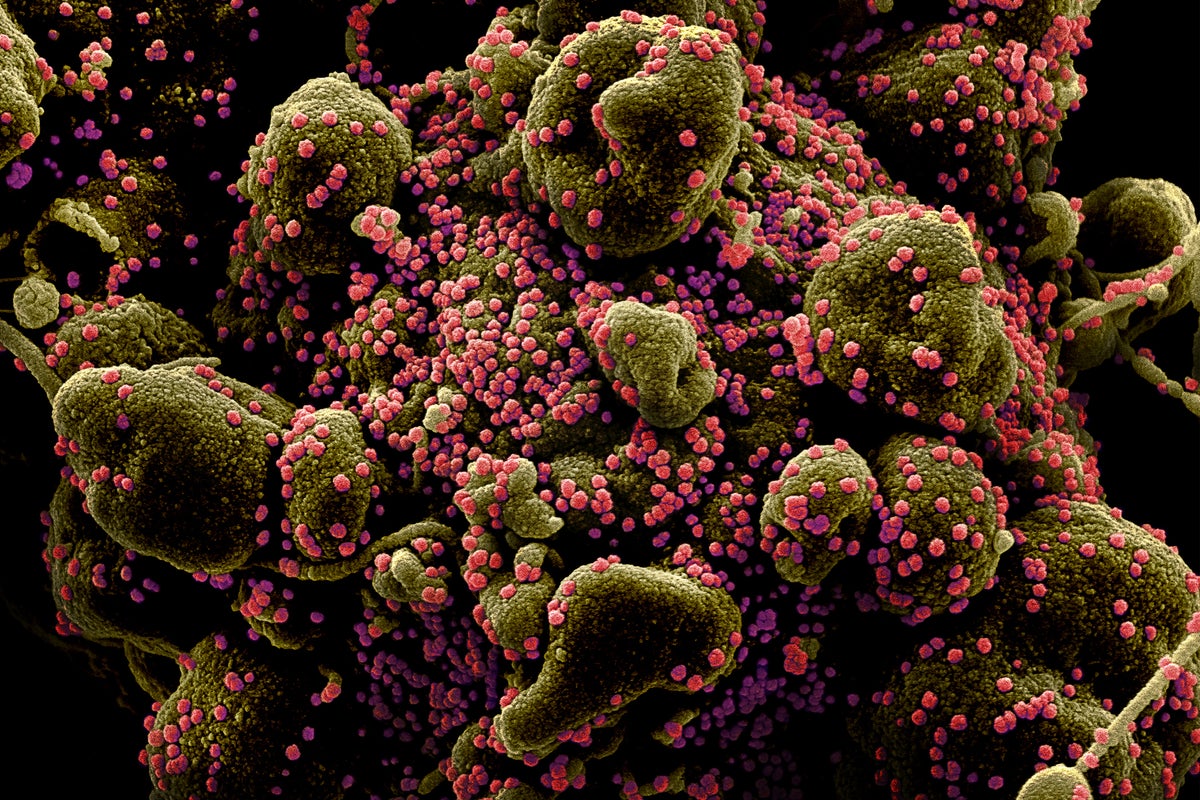
Medical Imaging Analysis and Diagnosis
Advanced image processing can be invaluable for patient diagnosis. Custom software can create accurate images to visualize internal body structures. For example, CT scans and X-ray data can be used to model tumors and surrounding tissue to guide cancer treatment. Using scanned images and 3D renderings, oncologists can plan surgical procedures or better target radiation therapies.
Modeling the human heart, for example, reveals details about arteries, valves, and chambers. This can aid cardiologists in diagnosing congenital heart disease and determine the best protocols for treatment.
Using custom software enables the integration of AI algorithms that automate analysis and allows more precise measurements for procedures. 3D images can be used with computer-aided design (CAD) software to sculpt implants and prosthetics that can be produced using a 3D printer.
Images can also be stored using a Picture Archiving and Communication System (PACS), which eliminates the need for physical images and X-rays and makes it easier to share images for collaborative diagnosis. For example, orthodontists and oral surgeons use computer models of patients’ teeth and jaws to plan out dental implants and the placement of braces.
More custom software and data integration will be needed as medical imaging becomes more sophisticated. Medical imaging devices will need to share data, so new software that adheres to DICOM (Digital Imaging and Communications in Medicine) and other standards will be required. Software experts are already developing new strategies to apply AI to medical images for automated detection of disease and anomalies and to assist with diagnoses. Digital imaging data also will need to be shared with different medical equipment and systems for greater efficiency and to improve patient care. Specialized software will also streamline clinical workflows, making sharing images, making notations, and reporting results easier.
Realistic Medical Training
Virtual and augmented reality experience give trainees hands-on experience practicing surgeries and understanding anatomy. These 3D experiences are safe and replicable, allowing students of all skill levels to gain experience developing critical skills. The more sophisticated the models, the more realistic the experience. 3D models are also ideal for training physicians and therapists to use new equipment.
Stanford Medicine’s Neurosurgical Simulation and Virtual Reality Center uses patient-specific 3D virtual reality models for surgical training and planning. These models, created from imaging scans like MRIs and CTs, allow medical trainees to practice complex procedures in an immersive environment. This technology enhances their confidence and decision-making skills while also being used to educate patients and assist surgeons with pre-operative planning.
Better Patient Education
Doctors increasingly use 3D models for patient education, explaining complex medical procedures and treatments. Apps also inform patients about their prescriptions. For example, one AR app allows patients to scan their medications to reveal overlays with information about dosages and side effects. Using imaging for drug education has been shown to improve medication adherence by 30%.
3D imaging continues to advance healthcare, and more. Medical institutions and practices are already taking advantage of the latest innovations, such as AI, AR/VR, robotics, and 3D printing. As patients require personalized care, more customized software will be needed to make healthcare more efficient and personalized. This trend will only continue, with those failing to embrace new technologies falling behind.
About Nik Froehlich
Nik Froehlich is the CEO and Founder of Saritasa. His passion for technology and the incredible enhancements it brings to our everyday lives inspired him to start Saritasa in 2005. He recognized that many businesses are often afraid to adopt new technologies and sought a way to bridge the gap between innovation and business. Under his leadership, Saritasa has helped numerous healthcare organizations implement custom software solutions that transform patient care and clinical operations.





























































































.jpg?#)




































