Emerging Technologies that are Driving Significant Innovations in Digital Health and Reshaping Patient Care Delivery
Countless people and organizations are currently striving to invent and improve technologies to help propel healthcare into a brighter future. But which of these technologies is starting to make a noticeable impact? What emerging technologies are driving the most significant innovations in digital health, and how are they reshaping patient care delivery? We reached out […]

Countless people and organizations are currently striving to invent and improve technologies to help propel healthcare into a brighter future. But which of these technologies is starting to make a noticeable impact? What emerging technologies are driving the most significant innovations in digital health, and how are they reshaping patient care delivery? We reached out to our brilliant Healthcare IT Today Community for their insights into this topic. The following are their answers.
James Lu, CEO at Helix
The year 2024 marked a significant milestone in genomic medicine, as large-scale outcomes data began to demonstrate the value of integrating genomic screening into standard care protocols. Projections indicate that by 2025, over one million individuals nationwide will undergo genomic screening through various approaches. This trend is expected to continue as health systems increasingly utilize these genomic tools to improve long-term patient outcomes, reduce healthcare costs, and enable more proactive and precise health management strategies.
As genomic integration becomes more prevalent among health systems, a broader paradigm shift is occurring. Both the health insights derived from genomic data and the subsequent care management protocols are becoming increasingly available within the primary care delivery system. This integration is poised to substantially reduce the care gaps that often result from self-directed or consumer-oriented genomic testing solutions. By embedding genomic insights directly into the healthcare delivery framework, providers can more effectively translate genetic information into actionable clinical interventions, ensuring a more comprehensive and coordinated approach to patient care.
Ion Hatzithomas, CEO at RenderHub
In recent years, the healthcare industry has witnessed a groundbreaking transformation driven by innovations in 3D visual technologies. These advancements — specifically in the areas of 3D printing, bioprinting, mobile 3D imaging, VR/AR for surgeries, and 3D medical animations — are solving the critical challenges faced by healthcare practitioners in diagnostics, treatment, education, and patient care.
From improving diagnostic speed and accuracy to personalizing prosthetics, implants, and bioprinted tissues, these technologies are proving themselves to be increasingly vital. Additionally, as AI continues to advance, the healthcare industry could soon see breakthroughs such as 3D imaging systems that can enhance diagnostic capabilities by providing predictive insights based on large datasets, allowing physicians to identify diseases early and suggest the most effective treatments.
By embracing the potential of 3D visual technology, medical professionals can continue pushing the boundaries of what’s possible in healthcare.
Elevsis Delgadillo, SVP, Customer Success at KeenStack
The integration of AI into nearly all technology services surrounding patient care is set to drive some of the most significant innovations in healthcare. Solutions like DAX Express and Suki leverage conversational and ambient AI to generate clinical notes rapidly and accurately. By streamlining the documentation process, these tools enable healthcare providers to focus more on patient engagement rather than spending the majority of an appointment typing on a keyboard. AI-powered physician assistant tools directly address clinician burnout, freeing doctors to provide more effective and personalized care.
Charles Jaffe, MD, PhD, FHL7, CEO at HL7 International
Interoperability is the backbone of digital health innovation. As AI, remote monitoring, and predictive analytics reshape patient care, the ability to seamlessly exchange data across systems is more critical than ever. Standards like HL7 FHIR are making real-time data access a reality, enabling better care coordination, reducing administrative burden, and fueling innovation. We are seeing a shift from fragmented, siloed information to a more connected ecosystem that supports personalized, data-driven decision-making. The future of digital health will be defined by how well we can bridge data silos and ensure that health information flows securely, efficiently, and in a way that truly improves patient outcomes.
Shelly Disser, DBA, Vice President, Innovation and Collaboration Team at MediQuant
An interesting technology that is driving innovation in digital health today is a real-time location service, which is being used to track patient and equipment locations within the hospital. There were several companies at VIVE showcasing this technology. Not only would it save a great deal of time for tracking patients, staff, and equipment, but it would also collect data that can be used to monitor patient and equipment timings and efficiencies, help with accident prevention, and the like.
Other digital health innovations, such as smart and wearable devices and telehealth to monitor patient status, are having a direct impact on underserved areas. The internet, satellite, and cellular networks are becoming more available to rural areas and using these infrastructures as a taking-off point for expanding care to these populations is a logical next step.
Jordan Bazinsky, CEO at Intelerad
The most significant innovation in digital health is not any single emerging technology—it’s the integration of multiple advancements to build a more connected, efficient healthcare ecosystem. Single-point solutions often fail to meet the complex demands of the medical imaging industry. For example, combining cloud-based imaging with AI enhances diagnostic accuracy and efficiency, while pairing cloud-native PACS with strong cybersecurity measures safeguards patient data and strengthens trust. By uniting these technologies, healthcare providers can deliver faster, more secure, and more precise patient care. The future of medical imaging depends on integrated solutions that work together to improve patient care and outcomes and advance industry growth.
Jason Herzog, Co-Founder and CEO at Holon Health
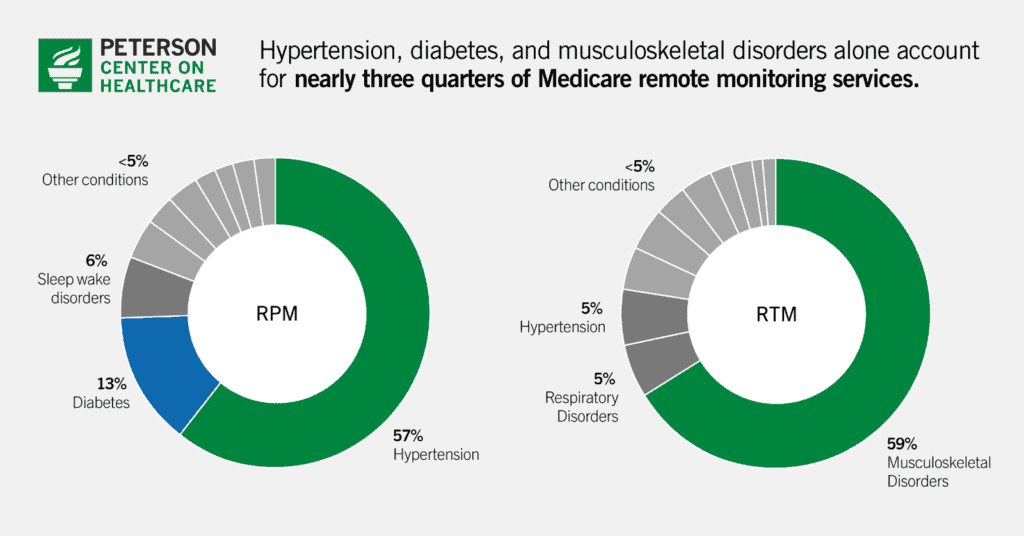
A handful of emerging technologies are sparking major innovations in digital health, with remote physiological monitoring (RPM) and remote therapeutic monitoring (RTM) leading the charge. These tools are revolutionizing patient care delivery by enabling near real-time connections between patients and providers, shifting healthcare from reactive fixes to proactive solutions, especially for those with chronic medical or mental health conditions. RPM can be a lifeline for managing chronic diseases—doctors can tweak meds or step in before a small issue becomes a hospital stay. RTM, meanwhile, keeps tabs on treatment progress, like how well someone’s sticking to their meds or coping with mental health challenges.
Digital solutions and mobile apps are helping keep patients engaged in their behavioral health treatment through daily therapeutic lessons and rewards, while handing providers real-time insights—like mood shifts or missed steps—that flag relapse risks early. For someone battling addiction, this could mean the difference between a timely check-in and a downward spiral. Together, RPM and RTM catch setbacks before they escalate, which is clutch for chronic conditions and mental health—data shows they can slash hospital readmissions by double digits for things like heart failure.
They widen access too; patients stuck in remote areas or with no ride to the clinic can still get top-tier care. And they cut costs—fewer ER visits and inpatient stays could save billions yearly. Add in AI diagnostics, telehealth, and secure data platforms like blockchain, and you’ve got a full-on transformation. AI crunches RPM data to predict trouble, telehealth ties it all together with virtual visits, and the result is care that’s more connected and patient-focused—less waiting, more doing.
Jeff Bennett, Chief Strategy and Innovation Officer at Modivcare
The expanded use of technology to support remote monitoring, including remote biometric data and survey-based collection devices, virtual care offerings, and digital engagement tools, is reshaping patient care by facilitating a care model designed to meet the unique needs of each patient balanced with the financial models of the payer responsible for the cost of the participant’s care. Data collected through in-home devices, filtered through the lens of a clinical team, allows providers and health plans to not only access ongoing biometric readings but also collect valuable types of health data through a trusted healthcare partner, such as health-related social needs information, to better understand the needs of their at-risk populations. Leveraging these insights can lead to stronger partnerships between payers and providers, enable earlier care interventions, reduce hospital readmissions and the associated cost of care, improve chronic disease management, and inform a more holistic approach. As adoption increases, these solutions will increasingly bridge gaps in care and help optimize resource allocation.
The integration of proactive and personalized monitoring technology also enables a more holistic system for care management through improved coordination between stakeholders and a curated, seamless experience for those in need of care. With the addition of a clinically-enabled support model, the resulting reduction of siloed information that’s traditionally collected across disparate sources leads to a uniformity that allows for consistent and extensive support across all environments, from a provider’s office all the way to the patient’s community and home. Providers also benefit from this unification of patient data, allowing access to comprehensive insights from primary care, behavioral health, social services, and beyond that enabling more personalized and informed decision-making for care teams to collaboratively improve healthcare outcomes.
Salvatore Viscomi, Co-Founder and CEO at Carna Health
Across industries, AI and predictive technologies are transforming decision-making and how we approach challenges, and healthcare is no exception. These innovations are driving a major shift toward more personalized treatments in digital health. By leveraging diverse patient data, they are enhancing health equity, enabling more precise interventions, and expanding access to tailored care across different demographics and regions.
Specifically, the rise of remote monitoring tools and wearable devices tracking real-time health metrics can empower patients, particularly in underserved areas, to take control of their health, while also reducing administrative burdens. By automating data collection and analysis, these technologies support timely interventions and enhance patient outcomes, which could help mitigate health disparities and reduce physician burnout. Rapid screening tools, for example, facilitate the early identification of chronic diseases such as chronic kidney disease (CKD). Social and economic inequities drive disparities in CKD prevalence globally, but affordable digital health technologies provide an opportunity to improve CKD outcomes, especially in lower-income, resource-limited regions.
Predictive machine learning (ML) is also transforming care by upskilling the workforce and shifting the focus from treatment to prevention, significantly reducing costs and physician burnout. Upskilling refers to enhancing the skills of healthcare professionals to ensure they can effectively utilize new technologies and manage evolving healthcare challenges. By equipping nurses, pharmacists, and primary care doctors with AI-powered tools, healthcare providers can streamline workflows, enhance patient-centric care, and improve treatment precision through ML-driven personalization, supporting patients beyond diagnosis for better health outcomes. Overall, as these trends evolve, the digital health landscape is set to become more interconnected, emphasizing holistic, patient-centered care that not only addresses immediate health concerns but also allows physicians to focus on offering the best care and promote long-term wellness.
Camille Cook, Senior Director, Healthcare Strategy & Innovation at LexisNexis Risk Solutions
Emerging technologies like AI, telemedicine, wearables, tokenization, and data enrichment are reshaping patient care, with significant implications for clinical trials and research, especially in terms of equity and access. Tokenization ensures that patient data is securely shared in clinical trials, maintaining privacy while allowing researchers to access important data for more accurate, inclusive study outcomes. Data enrichment improves the quality of clinical research by providing a fuller picture of patient health, which can be critical in studies aiming for diverse and representative populations. Consumer consent engines empower patients to control their own data, ensuring they are fully informed and their privacy is respected, which is particularly important in ensuring ethical participation from vulnerable groups.
To truly maximize the impact of these innovations, we must prioritize equitable access across all populations. When vulnerable groups, such as those in low-income or underserved communities, have access to these technologies, clinical trials become more inclusive, offering insights that are representative of a broader spectrum of society. Ensuring equal access to digital health technologies—whether through subsidies, policies, or other measures—helps level the playing field. This approach isn’t just about making technology available; it’s about ensuring that these innovations are used responsibly, ethically, and transparently, with patients’ consent and control over their data to maintain trust. Supporting the most vulnerable populations with equitable access to telemedicine, wearables, and secure data-sharing platforms benefits society as a whole. By prioritizing those most at risk, we foster a healthier, more inclusive society.
Dr. Bala Hota, SVP & Chief Informatics Officer at Tendo
Artificial intelligence, predictive analytics, and interoperability solutions are transforming digital health. AI enhances diagnostics, automates administrative tasks, and personalizes treatment plans. Predictive analytics help providers anticipate patient needs, while interoperability platforms enable seamless data sharing, improving care coordination and patient outcomes. A great example of this is how healthcare providers can better understand and impact their quality ratings from organizations like U.S. News and CMS. AI and predictive analytics enable organizations to recognize and document areas where they are already excelling, while also identifying gaps and opportunities for improvement. By leveraging these insights, health systems can optimize performance measures, enhance patient outcomes, and ensure they receive appropriate recognition for delivering high-quality care.
Huge thank you to everyone who took the time out of their day to submit a quote! And thank you to all of you for taking the time out of your day to read this article! We could not do this without all of your support.
What emerging technologies do you think are driving the most significant innovations in digital health, and how do you think they are reshaping patient care delivery? Let us know over on social media, we’d love to hear from all of you!





























.jpg)











































































![The breaking news round-up: Decagear launches today, Pimax announces new headsets, and more! [APRIL FOOL’S]](https://i0.wp.com/skarredghost.com/wp-content/uploads/2025/03/lawk_glasses_handson.jpg?fit=1366%2C1025&ssl=1)
















