When Ignoring Artificial Intelligence Becomes Medical Malpractice
Medical malpractice claims, tragic patient outcomes, and preventable errors have long plagued our healthcare system, fueled by the inherent limitations of human clinicians. But there is a revolutionary force in medicine that has the power to transform these outcomes: artificial intelligence (AI). Despite AI’s proven ability to identify diseases with greater speed and accuracy than human experts, many healthcare providers ... Read More


Medical malpractice claims, tragic patient outcomes, and preventable errors have long plagued our healthcare system, fueled by the inherent limitations of human clinicians. But there is a revolutionary force in medicine that has the power to transform these outcomes: artificial intelligence (AI).
Despite AI’s proven ability to identify diseases with greater speed and accuracy than human experts, many healthcare providers are resisting its integration. This hesitation is no longer just a technological lag—it is an ethical and legal failure. As Jason Matzus, a prominent Pittsburgh medical malpractice lawyer, asserts: “The refusal to adopt AI in initial diagnostic phases is not just a missed opportunity; it’s a fundamental breach of a provider’s duty to deliver competent care. When a tool exists that can save lives, the choice not to use it borders on negligence.”
Every year, diagnostic errors contribute to up to 10% of patient deaths and 33% of malpractice claims, according to research. Misdiagnoses aren’t merely statistical failings; they devastate families and erode trust in medical institutions. Many of these errors occur in the early stages of care—a phase where AI excels.
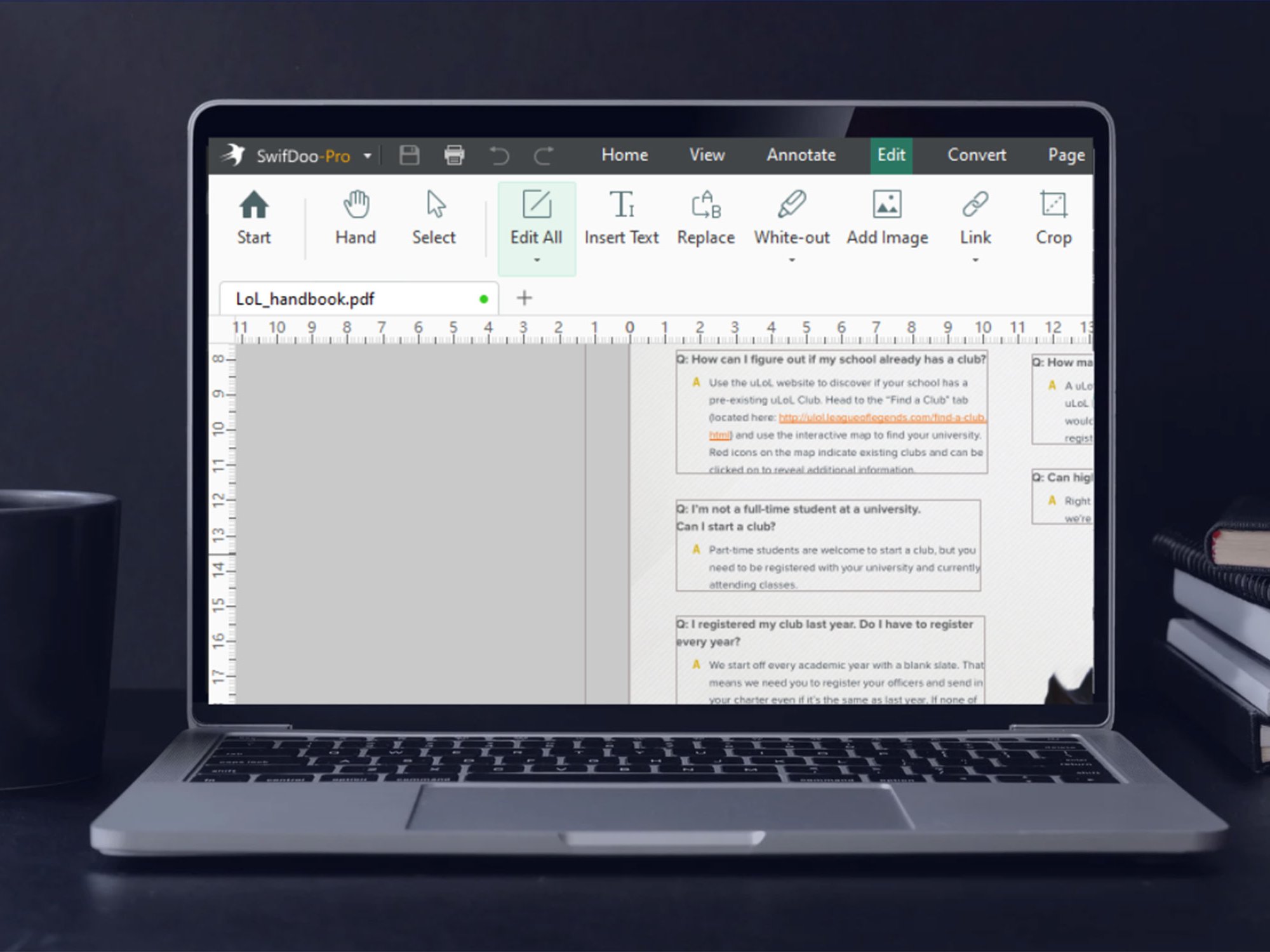
Here’s why AI makes so much sense today as a baseline preventative for medical malpractice: AI systems can analyze medical images, pathology slides, and patient histories with unprecedented precision and comprehensiveness. They detect patterns invisible to the human eye, offering real-time insights that guide clinicians to faster and more accurate conclusions. In radiology, for example, AI algorithms can pinpoint abnormalities in medical imaging with greater accuracy than even the most seasoned radiologists. In pathology, AI aids in detecting cancerous cells that human eyes might miss. AI systems can review the complete medical chart of a patient instantaneously so that no important clinical information or concerning trends get missed to help ensure that the patient gets a correct diagnosis.
Central to the medical profession is the ethical principle of beneficence—the obligation to act in the best interest of patients. By improving diagnostic accuracy and reducing the risks of misdiagnoses, AI fulfills this principle. Its omission, on the other hand, is tantamount to choosing mediocrity when excellence is available. Beyond ethics, the legal implications are profound. Failing to adopt AI where it is readily available and validated is increasingly being viewed as a deviation from the standard of care.
Matzus warns: “As courts recognize the transformative potential of AI, we will see cases where the absence of AI in diagnostic workflows is classified as negligence. Healthcare providers who ignore this reality are exposing themselves to significant legal risks.” The implications are stark. Consider a patient presenting with ambiguous symptoms that could be clarified by AI. If a clinician’s failure to use AI leads to harm, a malpractice claim may not simply focus on the human error but on the conscious decision to ignore available technology.
Critics of AI adoption point to high costs, integration difficulties, and ethical concerns like algorithmic bias. These challenges are valid but solvable. The initial expense of AI implementation pales in comparison to the long-term savings—not just in dollars but in lives. Outdated infrastructure can be modernized, and regulatory frameworks can ensure that AI tools remain transparent and fair. Moreover, AI is not replacing doctors; it is enhancing them. Clinicians will always hold the ultimate responsibility for patient care. The role of AI is to augment their decision-making, reducing cognitive biases and errors while empowering them with data-driven insights.
For AI to achieve its potential, systemic changes are required. Healthcare systems must invest in training clinicians to use AI tools effectively, regulators must establish clear guidelines for its adoption, and technology developers must collaborate with providers to ensure usability and reliability. The evidence is irrefutable. AI saves lives, improves care, and minimizes errors. Its omission is no longer defensible—ethically, professionally, or legally. The future of medicine demands that we embrace AI, not as a luxury but as a standard of care. As we stand on the brink of this transformative era, the question is not whether we can afford to integrate AI, but whether we can afford not to.
About Aron Solomon
A Pulitzer Prize-nominated writer, Aron Solomon, JD, is the Chief Strategy Officer for AMPLIFY. He has taught entrepreneurship at McGill University and the University of Pennsylvania, and was elected to Fastcase 50, recognizing the top 50 legal innovators in the world. Aron has been featured in Newsweek, The Hill,, Fast Company, Fortune, Forbes, CBS News, CNBC, USA Today, ESPN, TechCrunch, BuzzFeed, Venture Beat, The Independent, Fortune China, Abogados, Today’s Esquire, Yahoo!, ABA Journal,Law.com,The Boston Globe, and many other leading publications across the globe.