Collaboration Across the Healthcare Ecosystem: A Key to Revenue Cycle Success
The following is a guest article by Frank Forte, CEO at EnableComp The healthcare revenue cycle has never been more complex. As electronic health record (EHR) systems become nearly universal and interoperability initiatives gain momentum, many healthcare providers assume their revenue cycle challenges are solved. However, the reality is more nuanced, especially regarding complex claims […]
The following is a guest article by Frank Forte, CEO at EnableComp
The healthcare revenue cycle has never been more complex. As electronic health record (EHR) systems become nearly universal and interoperability initiatives gain momentum, many healthcare providers assume their revenue cycle challenges are solved. However, the reality is more nuanced, especially regarding complex claims management.
The Evolution of Healthcare Technology
The healthcare industry has witnessed a dramatic technological transformation over the past 15 years. In 2008, 9% of hospitals and 17% of office-based physicians used EHR systems. By 2021, these numbers had soared to 96% and 78%, respectively. This digital revolution has streamlined many aspects of healthcare delivery and billing, but significant challenges remain, especially in complex areas of the revenue cycle.
The Complex Claims Challenge
While EHR systems excel at managing routine tasks and standard commercial claims processing, they often fall short when handling complex claims that involve multiple payers, intricate coding requirements, varying reimbursement rules, and frequent denials. The challenges become particularly acute when dealing with specialized claims outside typical commercial insurance processing, such as for military payers.
The scope of these challenges is striking, with approximately 60% of workers’ compensation claims being initially sent to incorrect carriers, leading to significant processing delays and increased administrative costs. Veterans Administration (VA) claims face similar hurdles, with about 13% being denied due to various technical issues, including timely filing violations, coding errors, authorization problems, carrier selection mistakes, and eligibility verification failures. The motor vehicle accident claims landscape isn’t much better, with roughly 20% of claims being misdirected and requiring resubmission. Perhaps most concerning is that between 25% and 33% of out-of-state Medicaid claims are never filed due to enrollment complications.
These statistics underscore a deeper problem: the increasing complexity of healthcare billing and reimbursement has outpaced the capabilities of standard systems and processes. Each specialized claim type has its own rules, requirements, and potential pitfalls. Special expertise in handling such claims is needed to help providers go beyond the basics to manage even the most complex aspects of the revenue cycle more reliably and efficiently.
The Need for Ecosystem Collaboration
These challenges highlight why collaboration across the healthcare ecosystem—involving hospitals, payers, third-party administrators, and specialized service providers like EnableComp—is crucial for success. The complexity of modern healthcare revenue cycle management demands a multifaceted approach that draws on the strengths of various stakeholders.
At the heart of successful collaboration is specialized expertise, which most health systems are challenged to provide. Complex claims require deep knowledge of specific payer guidelines, state regulations, and documentation requirements that no single organization can realistically maintain across all areas. Complex claims typically account for 5% or less of a hospital’s gross patient revenue, making building and retaining specialized staff challenging and expensive. By forming strategic partnerships, healthcare organizations can access the specific expertise needed for different claim types while focusing on their core competencies.
Technology integration forms another critical pillar of effective collaboration. While EHR systems provide robust foundations for healthcare operations, they must interface effectively with various specialized systems and tools. This necessitates close cooperation between technology vendors, healthcare providers, and payers to ensure seamless data flow and process automation. The goal is to connect systems and create intelligent workflows that improve efficiency and accuracy across the revenue cycle.
Regulatory compliance represents a third crucial area where collaboration delivers significant value. Different payer groups have unique rules and regulations that require specific knowledge and careful attention to detail. Workers’ compensation claims, for example, demand specific expertise to avoid authorization errors, missed filing deadlines, and inaccurate coding. Through collaborative partnerships, organizations can share knowledge and best practices to ensure compliance and reduce denials across all claim types.
Building Effective Partnerships
The success of healthcare ecosystem collaboration depends heavily on how partnerships are structured and maintained. Effective data sharing and interoperability are the foundation, requiring secure and efficient clinical data exchange and administrative and financial information for proper claims processing. This comprehensive data sharing enables all stakeholders to make informed decisions and take appropriate actions promptly.
Communication proves equally vital to partnership success. Organizations must establish and maintain clear channels for regular dialogue between all parties. This ongoing communication helps prevent misunderstandings, expedites problem resolution, and ensures all stakeholders remain aligned on goals and challenges. Regular check-ins and status updates keep projects on track and allow quick adaptation when issues arise.
Process standardization represents another key element of successful partnerships, though it requires careful balance. Partners should work together to standardize processes, creating consistent workflows that enhance efficiency and reduce errors. However, they must be flexible enough to handle unique situations and complex cases requiring special attention. This balanced approach ensures that standardization is a tool for improvement rather than a rigid constraint.
The final piece of the partnership puzzle involves comprehensive performance monitoring. By regularly tracking and reporting key metrics, organizations can identify areas for improvement and ensure all partners are consistently meeting shared expectations. This data-driven approach supports the continuous improvement of collaborative efforts and helps demonstrate the value of partnerships to all stakeholders.
The Future of Healthcare Collaboration
As healthcare continues to evolve, the importance of ecosystem collaboration will only grow. Emerging technologies like artificial intelligence and machine learning will create new opportunities for automation and efficiency, but successful implementation will require even closer cooperation between stakeholders.
The key to success is recognizing that no organization can excel at everything. By fostering partnerships that leverage each participant’s strengths, healthcare organizations can build more efficient, effective revenue cycle operations that benefit all stakeholders –– most importantly, the patients they serve.
Complex claims management requires a collaborative approach that combines the strengths of various healthcare ecosystem participants. While technology provides the foundation, success depends on building effective partnerships that combine specialized expertise, advanced technologies, integrated systems, and standardized processes. As healthcare evolves, organizations embracing collaboration will be best positioned to thrive in an increasingly complex environment.
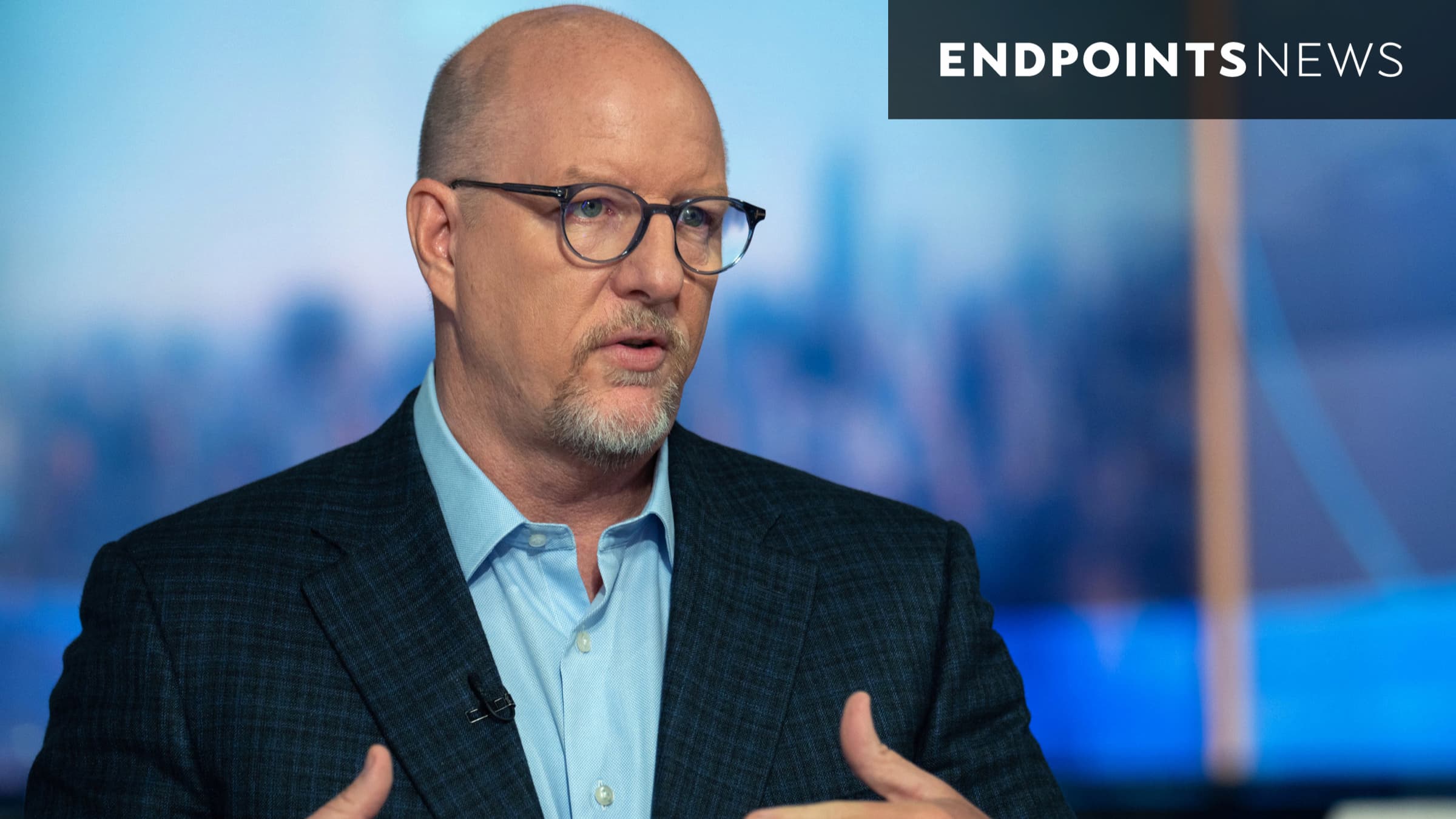
 About Frank Forte
About Frank Forte
As CEO at EnableComp, Frank Forte brings a wealth of experience and a proven track record in revenue cycle management and executive leadership, having most recently served as CEO at AnatomyIT and as a leader in cybersecurity and IT solutions for healthcare. Previously, he was Chief Commercial Officer and General Manager at Cloudmed Solutions, where he drove commercial strategy, scaled operations, and integrated multiple acquisitions. Forte has also held leadership roles in business development, operations, and strategy at several healthcare, services, and technology companies, including Emerson Electric Corporation.