AI in Primary Care: Reducing Burnout and Empowering Physicians
Primary care physicians struggle to process a novel’s worth of data on each of their patients, every day, under stressful conditions. As healthcare invests billions in fast-evolving AI solutions, I’m convinced that leveraging AI to expand automation and save time in healthcare won’t work unless we prioritize helping these doctors operate at the top of ... Read More


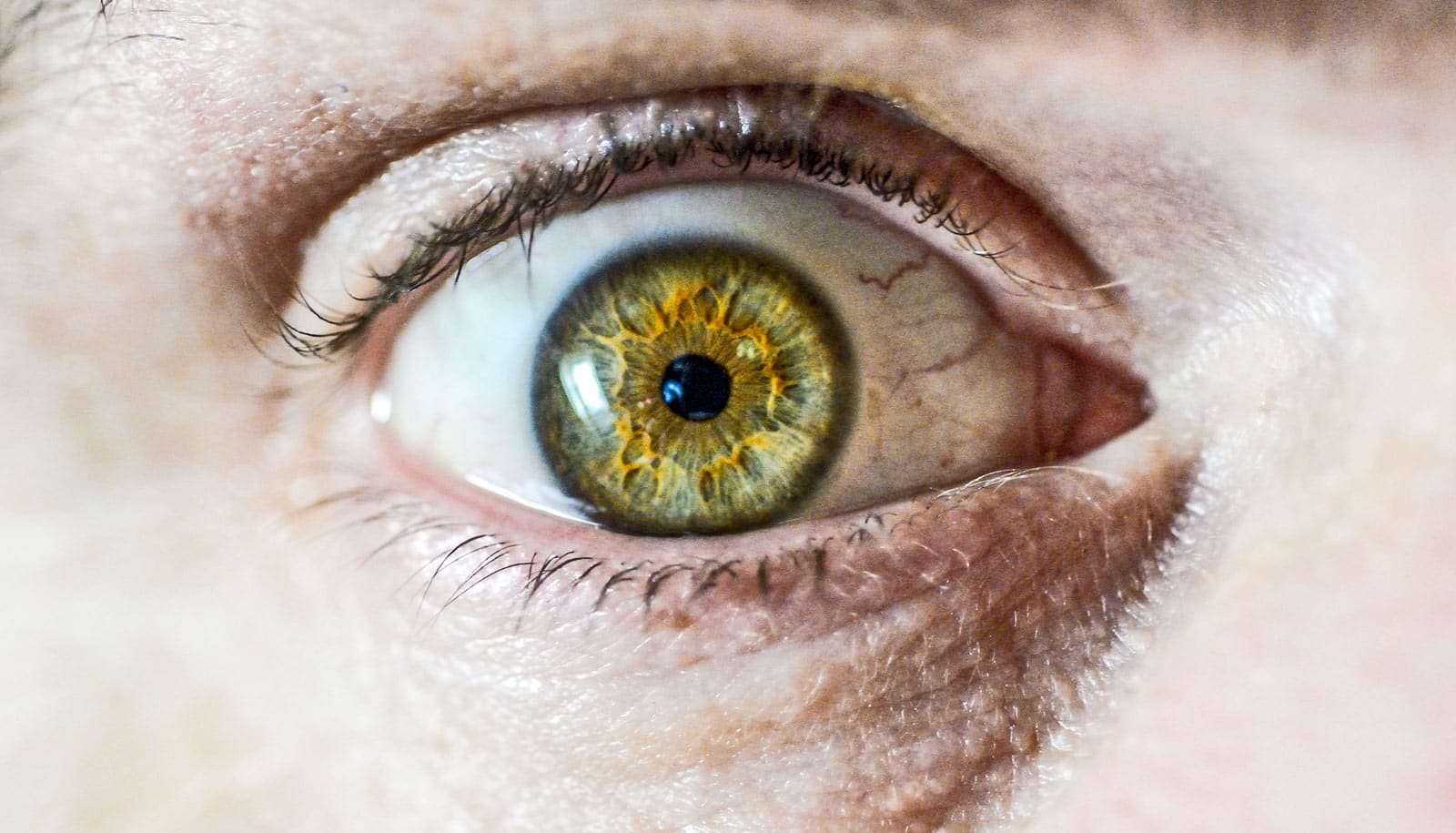
Primary care physicians struggle to process a novel’s worth of data on each of their patients, every day, under stressful conditions. As healthcare invests billions in fast-evolving AI solutions, I’m convinced that leveraging AI to expand automation and save time in healthcare won’t work unless we prioritize helping these doctors operate at the top of their license.
Every patient has a rich story. Primary care physicians are tasked with quickly finding and reviewing those personal stories in medical records, claims, mental health, and other electronic data while coordinating treatment plans for multitudes of patients.
These growing volumes of patient data create opportunities for better care but also challenges. The doctors, for example, know that even when they deliver their best care, they can’t consider 100 percent of a patient’s history, related medical literature, insurance, and other important information, like social determinants of health, in a 20-minute visit. They simply don’t have the time.
This grind – I view it as a moral injury over time – explains why the much-discussed epidemic of burnout in healthcare is especially acute among primary care physicians. According to the Association of American Medical Colleges, the US faces a shortage of as many as 40,000 primary care physicians by 2036. That’s almost half of the total shortage of doctors forecast for the same period.
New patient waiting periods are already at an all-time high – nine months or longer in some states. Unless healthcare innovators develop solutions, these challenges will overcome the industry. More people, especially a large cohort of older patients, will be competing for fewer doctors’ time, resulting in worse health outcomes due to untreated chronic illnesses.
Get ready for AI
There is a supply and demand gap, and that gap is widening with time. AI solutions hold the potential to help address the gap by making our clinicians more efficient and effective without them giving up control of the patient’s healthcare journey.
As chief health information officer at a major American healthcare system, I worked with doctors who studied for years to deliver care at the top of their license, not wonder what they might have found in the novels of data at their fingertips if they only had time to read them closely.
I recently joined a health AI company because I believe AI is the only solution on the horizon that can deal with this perfect storm of exponential data, condition complexity, and clinician shortage. I believe the future of healthcare lies in combining real-world clinical expertise with AI, creating a synergy that is greater than the sum of its parts. AI can help significantly if used wisely.
AI is ideally suited to help in primary care today because the doctor’s value is not their level of specialization in one area but rather their broad knowledge across specialties and their ability to make good care decisions with the information available. But leveraging automation and saving time can’t come at the expense of what primary care physicians need to do their best work – the most relevant patient insights at their fingertips.
Four principles to help primary care physicians deploy AI
Tools that combine clinical, social, and behavioral data with predictive AI and generative AI will increasingly help primary care physicians understand their patients’ statuses, obtain real-time recommendations to address their conditions, and ask “what-ifs” to help doctors work faster and – importantly – more confidently.
Strong collaborations between clinicians and AI that hew to four principles at the outset will help health systems regain time and capacity as they seek to take advantage of these tools.
First, everyone in healthcare must admit there is still a lot of hard work to accomplish before AI starts solving our time and staffing constraints.
Second, hard work always involves risk; nobody should be alarmed when changing the status quo requires disruption.
Third, new AI solutions must incorporate and reflect the experiences of the teams that will deploy them.
Fourth, AI should never replace clinicians; it should help clinicians comb through the data that they otherwise cannot or will not access to leverage the benefits.
Labor and benefits
Healthcare leaders shouldn’t pursue automation or other innovations for their own sake. They should think practically.
To start, AI today should help primary care physicians perform the routine labors of medicine that do not directly require the intervention of a licensed clinician: hunting through documents, managing referrals and follow-ups, determining patient complexity, recommending specialists with appropriate suggested timeframes and channels, and coordinating between channels at the right times while tracking labs, orders, and prescriptions.
These tasks are a key source of burnout in primary care – disrespecting the expertise by piling up tedious work that could be automated or moved to a more appropriate level of expertise. They spend too much time on these tasks today. Many have fled the vocation to avoid this non-clinical work that now burdens every care interaction.
At the same time, AI brings an intelligent assistant to other responsibilities like providing early disease detection, supplying rationales for the next best clinical actions, and ensuring all team members share the same recommendations and guidelines on care.
Less cognitive burden, higher quality of care, and spending more time on patients and orchestrating care – unleashing physicians to practice at the top of their license – should be the key indicators of whether the technology is working.
Final goals and bonuses
The final goal is the quadruple aim of better care experiences, better outcomes, better use of resources, and better conditions for caregivers. AI must help reduce wait times, ensure patients take the next steps in their care plan at the right time, slow disease progression, empower doctors to manage their patients’ care proactively, streamline administration, and improve clinician satisfaction, retention, and recruitment.
The bonus is cost control. Healthier patients who receive high-quality care through AI-empowered workflows will drive better patient satisfaction and doctor retention. Increased quality time and access lead to larger market shares and capture of downstream care, too. Improved STARS and HEDIS quality measures usually follow.
Primary care physicians, IDNs, and health systems have choices to make about confronting the challenges now facing primary care. They can either watch as current trends continue or empower the best, most caring professionals among us to keep everyone healthier and happier.
About Ed Glynn
Ed Glynn, MD, MBA, FAAFP, is Chief Clinical Officer at RhythmX AI, an SAIGroup company.