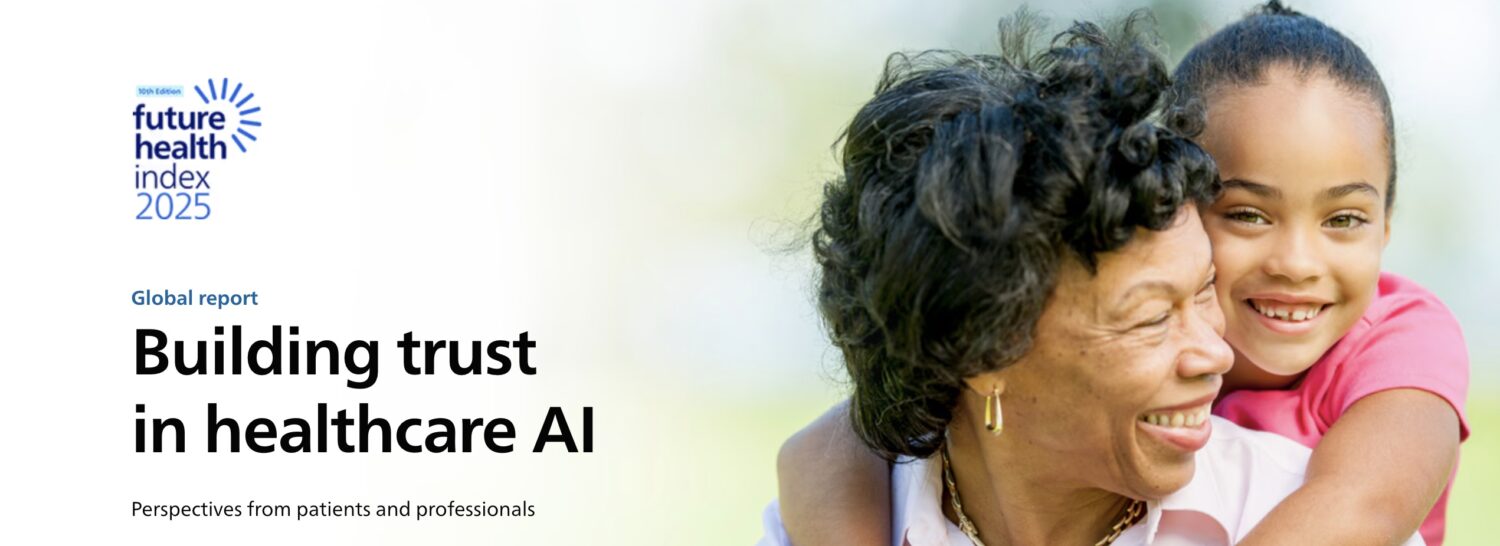
Philips’ Future Health Index 2025 Reveals Healthcare Strain, AI Promise, and Critical Trust Gaps
What You Should Know: – Philips, a global leader in health technology released its 10th annual Future Health Index (FHI) report. The FHI 2025 Report, the largest global survey of its kind analyzing the pressing concerns of both healthcare professionals and patients, paints a stark picture of growing strain on healthcare systems worldwide. – While ... Read More

What You Should Know:
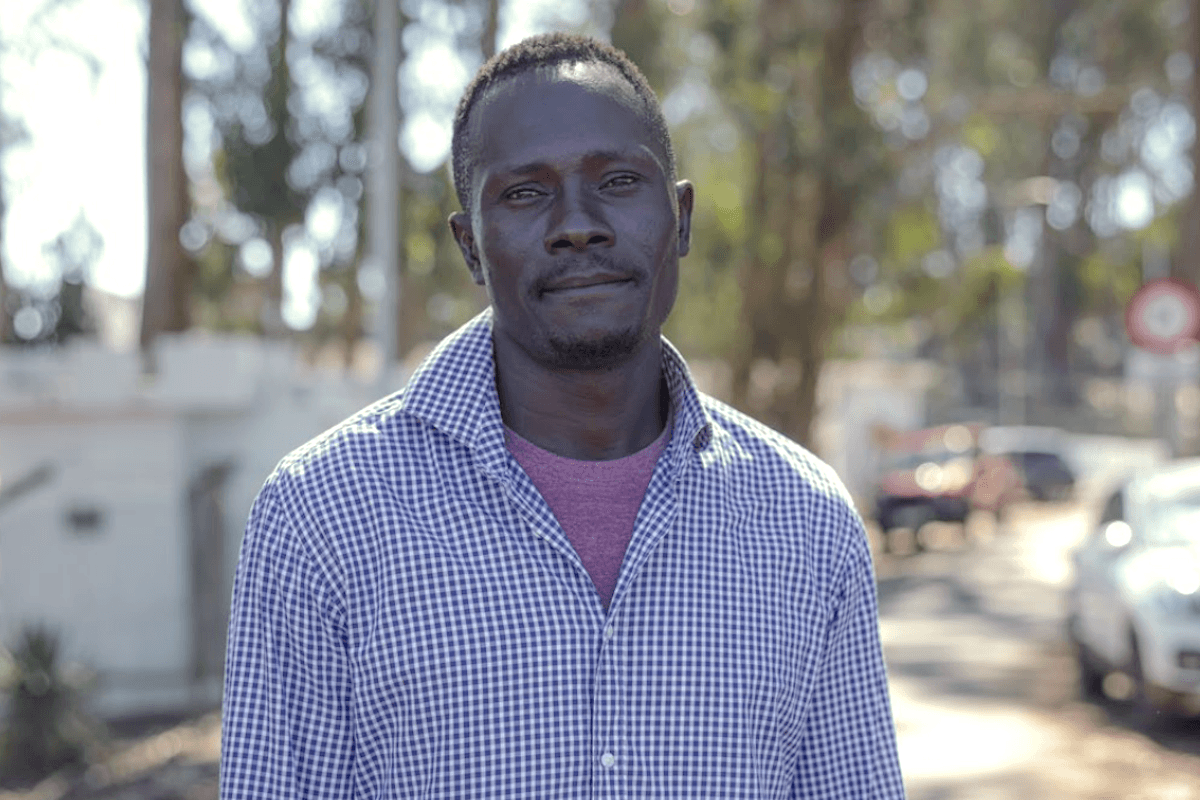
– Philips, a global leader in health technology released its 10th annual Future Health Index (FHI) report. The FHI 2025 Report, the largest global survey of its kind analyzing the pressing concerns of both healthcare professionals and patients, paints a stark picture of growing strain on healthcare systems worldwide.
– While artificial intelligence (AI) shows significant promise for transforming care delivery, the report highlights that substantial gaps in trust threaten to impede progress just when innovation is most urgently needed.
– The comprehensive report surveyed nearly 2,000 healthcare professionals and patients across 16 countries, offering deep insights into the challenges and opportunities facing global health.
Healthcare Systems Under Unprecedented Pressure: Long Waits and Worsening Outcomes
The FHI 2025 report underscores the escalating crisis of patient access and its dire consequences. “The need to transform healthcare delivery has never been more urgent,” stated Carla Goulart Peron, M.D., Chief Medical Officer at Philips. “In more than half of the 16 countries surveyed, patients are waiting nearly two months or more for specialist appointments, with waits in Canada and Spain extending to four months or longer.”
These delays are not without severe repercussions. The report reveals that 33% of patients have experienced a worsening of their health due to delays in seeing a doctor, and more than one in four (25%) end up hospitalized as a result of long wait times. Dr. Peron added, “Cardiac patients face especially dangerous delays, with 31% being hospitalized before even seeing a specialist. Without urgent action, a projected shortfall of 11 million health workers by 2030 could leave millions without timely care.”
Clinician Burnout and Data Burdens Signal Need for Digital Relief
The administrative load on healthcare professionals is a major contributing factor to the system’s strain. More than 75% of healthcare professionals surveyed reported losing valuable clinical time due to incomplete or inaccessible patient data. Alarmingly, one-third of these professionals lose over 45 minutes per shift, which equates to approximately 23 full days a year lost for each professional.
“These inefficiencies amplify stress on already understaffed teams and contribute to burnout,” commented Gretchen Brown, RN, VP and Chief Nursing Information Officer at Stanford Health Care. “Recognizing this, as clinicians, we see AI as a solution and understand that delayed adoption can also carry major risks.”
The survey found that if AI is not implemented, clinicians harbor significant fears:
- 46% fear missed opportunities for early diagnosis and intervention.
- Another 46% anticipate growing burnout from the burden of non-clinical tasks.
- 42% worry about an expanding patient backlog, further exacerbating wait times.
AI’s Promise Tempered by Significant Trust Gaps
While healthcare professionals are generally optimistic about AI’s potential, the FHI 2025 report identifies a critical trust gap, particularly with patients. The survey found that 34% more clinicians see the benefits of AI compared to patients, with optimism notably lower among patients aged 45 and older.
Even among clinicians, skepticism persists. Although 69% report being involved in the development of AI and digital technology, only 38% believe these tools currently meet real-world clinical needs. Concerns around accountability for AI-driven errors are widespread, with over 75% of clinicians unclear about where liability lies. Data bias is another significant worry, as it carries the risk of deepening existing healthcare disparities if not proactively addressed.
“To build trust with clinicians, we need education, transparency in decision-making, rigorous validation of models, and the involvement of healthcare professionals in every step of the process,” Brown added.
The Path Forward: Embracing Human-Centric AI Integration
The report suggests a clear path forward, emphasizing that patients want AI to operate safely and effectively, reducing errors, improving outcomes, and fostering more personalized and compassionate care. For clinicians, trust in AI hinges on the establishment of clear legal and ethical standards, robust scientific validation, and continuous human oversight.
“To realize the full potential of AI, regulatory frameworks must evolve to balance rapid innovation with robust safeguards to ensure patient safety and foster trust among clinicians,” said Shez Partovi, Chief Innovation Officer at Philips. He envisions a future where AI significantly transforms healthcare: “By 2030, AI could transform healthcare by automating administrative tasks, potentially doubling patient capacity as AI agents assist, learn, and adapt alongside clinicians. To that end, we must design AI with people at the center—built in collaboration with clinicians, focused on safety, fairness, and representation—to earn trust and deliver real impact in patient care.”







































































































.jpeg?#)